Presentation Slides
Chinese Medicine Research Hub
Review Article
A 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important.
2022 Expert Review of Neurotherapeutics Role of acupuncture in the treatment of migraine
Endres HG, Diener HC, Molsberger A
Chinese Medicine Research Hub
Systematic Review
Dietary strategies, such as caloric restriction and ketogenic diets, can alleviate chronic pain and enhance quality of life.
2022 International Journal of Environmental Research and Public Health The Effectiveness of Intermittent Fasting, Time Restricted Feeding, Caloric Restriction, a Ketogenic Diet and the Mediterranean Diet as Part of the Treatment Plan to Improve Health and Chronic Musculoskeletal Pain: A Systematic Review
Cuevas-Cervera M, Perez-Montilla J, Gonzalez-Muñoz A, Garcia-Rios M, Navarro-Ledesma S
Chinese Medicine Research Hub
Systematic Review
Acupuncture can reduce pain and improve functional activities in patients with knee osteoarthritis, proving particularly beneficial for chronic sufferers and enhancing their quality of life.
2022 BioMed Research International Acupuncture for Knee Osteoarthritis: A Systematic Review of Randomized Clinical Trials with Meta-Analyses and Trial Sequential Analyses
Tian H, Huang L, Sun M, Xu G, He J, Zhou Z, Huang F, Liu Y, Liang F
Chinese Medicine Research Hub
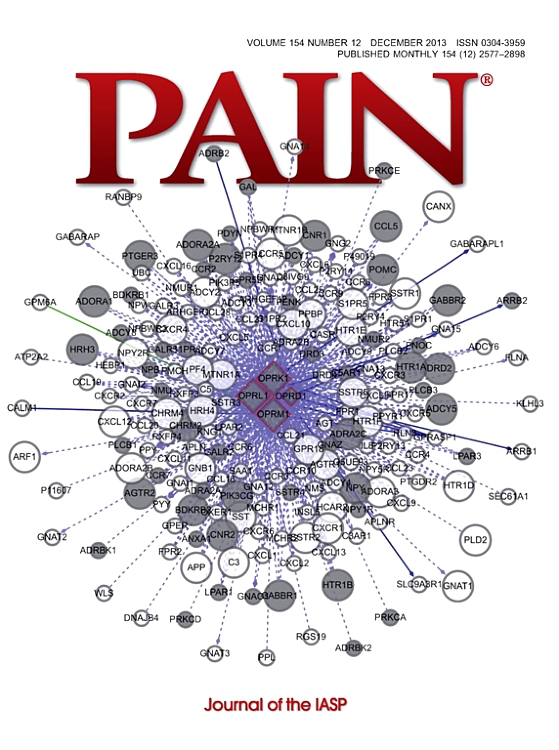
Network Pharmacology
The Gui Zhi-Shao Yao herb pair in traditional Chinese medicine potentially treats chronic pain, anxiety, and depression through interactions with nine key targets.
2022 Annals of Medicine A network pharmacology approach to predict potential targets and mechanisms of “Ramulus Cinnamomi (cassiae) – Paeonia lactiflora” herb pair in the treatment of chronic pain with comorbid anxiety and depression
Pan HT, Xi ZQ, Wei XQ, Wang K
Chinese Medicine Research Hub
Systematic Review
Acupuncture appears to have an effect on diabetic peripheral neuropathy, effectively improving nerve conduction and clinical symptoms.
2021 Journal of Clinical Pharmacy and Therapeutics Acupuncture treatment of diabetic peripheral neuropathy: An overview of systematic reviews
Yu B, Li M, Huang H, Ma S, Huang K, Zhong Z, Yu S, Zhang L.
Chinese Medicine Research Hub
Systematic Review
In the treatment of chronic pain with depression, acupuncture could not only achieve better clinical efficacy, but also have higher safety compared with conventional mediation therapy.
2020 Evidence-Based Complementary and Alternative Medicine Effect of Acupuncture on Chronic Pain with Depression: A Systematic Review
Yan B, Zhu S, Wang Y, Da G, Tian G
Chinese Medicine Research Hub
Review Article
Ginger, through various methods, exhibits promising pain reduction effects for conditions such as dysmenorrhea, muscle soreness, osteoarthritis, low back pain, and migraines.
2020 Phytotherapy Research Clinical trials on pain lowering effect of ginger: A narrative review
Rondanelli M, Fossari F, Vecchio V, Gasparri C, Peroni G, Spadaccini D, Riva A, Petrangolini G, Iannello G, Nichetti M, Infantino V, Perna S
Chinese Medicine Research Hub
Review Article
Pomegranate, due to its polyphenols, flavonoids and fatty acids, exhibits significant pain-relieving effects and could potentially be used as a treatment for various types of pain.
2020 Plants Pomegranate as a Potential Alternative of Pain Management: A Review
Guerrero-Solano JA, Jaramillo-Morales OA, Velázquez-González C, De la O-Arciniega M, Castañeda-Ovando A, Betanzos-Cabrera G, Bautista M
Chinese Medicine Research Hub
Systematic Review
Acupuncture reduced more headache days and the times of using painkiller and was more effective in reducing the frequency and degree of headache than western medicine and sham acupuncture.
2020 Pain Research & Management Effectiveness and Safety of Acupuncture for Migraine: An Overview of Systematic Reviews
Li YX, Xiao XL, Zhong DL, Luo LJ, Yang H, Zhou J, He MX, Shi LH, Li J, Zheng H, Jin RJ
Chinese Medicine Research Hub
Randomised Controlled Trial
Both individual and group acupuncture therapy delivered in primary care settings reduced chronic pain and improved physical function at 12 weeks.
2020 Journal of General Internal Medicine Individual vs. Group Delivery of Acupuncture Therapy for Chronic Musculoskeletal Pain in Urban Primary Care—a Randomized Trial
McKee MD, Nielsen A, Anderson B, Chuang E, Connolly M, Gao Q, Gil EN, Lechuga C, Kim M, Naqvi H, Kligler B
Chinese Medicine Research Hub
Systematic Review
There is growing evidence that acupuncture is just as effective and has fewer side effects than many of the standard pharmaceutical agents that are currently used.
2019 Headache Systematic Review: Acupuncture vs Standard Pharmacological Therapy for Migraine Prevention
Niushen Zhang, Tim Houle, Nada Hindiyeh, & Sheena K. Aurora
Chinese Medicine Research Hub
Review Article
Currently, acupuncture is considered to be a safe, helpful, and available alternative option for patients who have not responded to or complied with conventional pharmacotherapy.
2019 Neuropediatrics Acupuncture in Adult and Pediatric Headache: A Narrative Review
Doll, E., Threlkeld, B., Graff, D., Clemons, R., Mittel, O., Sowell, M. K.
Chinese Medicine Research Hub
Systematic Review
Acupuncture therapy is an effective and safe treatment for chronic pain-related insomnia.
2019 Evidence-Based Complementary and Alternative Medicine Acupuncture for Chronic Pain-Related Insomnia: A Systematic Review and Meta-Analysis
Fushui Liu, Jianyu You, Qi Li, Ting Fang, Mei Chen, Nana Tang, Xiaojun Yan
Chinese Medicine Research Hub
Randomised Controlled Trial
Strong electroacupuncture for at least two weeks improves chronic pain management in knee osteoarthritis patients better than weak or sham electroacupuncture.
2019 Arthritis Research & Therapy Effects of intensity of electroacupuncture on chronic pain in patients with knee osteoarthritis: a randomized controlled trial
Lv, Z., Shen, L., Zhu, B. et al.
Chinese Medicine Research Hub
Systematic Review
Acupuncture, regardless of the trial design, showed a positive effect on pain-related outcome measures for participants with diabetic peripheral neuropathy.
2019 Acupuncture in Medicine Acupuncture for the treatment of lower limb diabetic peripheral neuropathy: a systematic review
Nash J, Armour M, Penkala S
Chinese Medicine Research Hub
Systematic Review
We found good evidence that receiving acupuncture for chronic pain is better than not receiving treatment or being placed on a waiting list and reasonable evidence that it is better than conventional or usual care.
2019 Evidence-Based Complementary and Alternative Medicine Classic Chinese Acupuncture versus Different Types of Control Groups for the Treatment of Chronic Pain: Review of Randomized Controlled Trials (2000-2018)
Yan-Jiao Chen, Gabriel Shimizu Bassi, Yong-Qing Yang
Chinese Medicine Research Hub
Case Report
Acupuncture for cluster headache may be more effective if treated in the same way as has been shown effective for trigeminal neuralgia.
2018 Acupuncture in Medicine Acupuncture for Episodic Cluster Headache: A Trigeminal Approach
Simon Hayhoe
Chinese Medicine Research Hub
Systematic Review
There is potential of acupuncture combined with conventional treatment for treating female chronic pelvic pain.
2018 Evidence-Based Complementary and Alternative Medicine Acupuncture Treatment for Chronic Pelvic Pain in Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Sung SH, Sung ADM, Sung HK, An TEB, Kim KH, Park JK
Chinese Medicine Research Hub
Acupuncture therapy offered in the group setting was effective in reducing pain severity, pain interference, and depression in patients with chronic neck, back, or shoulder pain or osteoarthritis.
2018 Pain Medicine Acupuncture Therapy in a Group Setting for Chronic Pain
Benjamin Kligler, Arya Nielsen, Corinne Kohrherr,, Tracy Schmid, Eve Waltermaurer, Elidania Perez, Woodson Merrell
Chinese Medicine Research Hub
Systematic Review
Patients in both group and individual acupuncture study arms valued the pain relief, improved quality of life, and relaxation experienced during acupuncture.
2018 The Journal of Alternative and Complementary Medicine "It's Better in a Group Anyway": Patient Experiences of Group and Individual Acupuncture
Chuang, E., Hashai, N., Buonora, M., Gabison, J., Kligler, B., & McKee
Chinese Medicine Research Hub
Systematic Review
Acupuncture has a clinically relevant effect on chronic pain that persists over time. Referral for acupuncture treatment is a reasonable option for chronic pain patients.
2017 The Journal of Pain Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis
Vickers, Andrew J. et al.
Chinese Medicine Research Hub
Meta-Analysis
The existing evidence suggests that most acupuncture therapies, including acupuncture combined with other therapies, are effective in decreasing pain and in improving physical function.
2017 Pain Physician Acupuncture for Myofascial Pain Syndrome: A Network Meta-Analysis of 33 Randomized Controlled Trials
Li X, Wang R, Xing X, Shi X, Tian J, Zhang J, Ge L, Zhang J, Li L, Yang K.
Chinese Medicine Research Hub
Systematic Review
Patients with chronic pain can generally be reassured that treatment effects persist after a course of treatment with acupuncture.
2017 Pain The persistence of the effects of acupuncture after a course of treatment: a meta-analysis of patients with chronic pain
MacPherson, H; Vertosick, E.A; Foster, N.E; Lewith, G; Linde, K; Sherman, K.J; Witt, C.M; Vickers, A.J
Chinese Medicine Research Hub
Systematic Review
The programme of research found that acupuncture was more effective than usual care and sham acupuncture for chronic pain, that it was one of the more clinically effective physical therapies for osteoarthritis and that it showed benefits in the treatment of depression.
2017 Programme Grants for Applied Research Acupuncture for chronic pain and depression in primary care: a programme of research
MacPherson H, Vickers A, Bland M, et al.
Chinese Medicine Research Hub
Randomised Controlled Trial
A 14-session course of needling at Fengchi is relatively safe for treating posterior circulation ischemia with vertigo.
2016 Neural Regeneration Research Safety of different acupuncture manipulations for posterior circulation ischemia with vertigo
Wen Y, Zhang C, Zhao Xf, Deng Sz, He S, Huang Lh, Tian G, Meng Zh
Chinese Medicine Research Hub
Systematic Review
Clinicians may consider Tai Chi as a viable complementary and alternative medicine for chronic pain conditions.
2016 Scientific Reports Tai Chi for Chronic Pain Conditions: A Systematic Review and Meta-analysis of Randomized Controlled Trials
Kong, L., Lauche, R., Klose, P. et al.
Chinese Medicine Research Hub
Systematic Review
The majority of trials demonstrate a positive effect of acupuncture over control condition in the treatment of neuropathy.
2015 Neurology Effects of Acupuncture on Neuropathic Pain: A Systematic Review and Meta-analysis
Alexandra Dimitrova, Charles Murchison, Barry Oken
Chinese Medicine Research Hub
Randomised Controlled Trial
Improvement in post traumatic stress disorder severity was significantly greater among those receiving acupuncture than in those receiving usual PTSD care.
2014 Medical Care Randomized effectiveness trial of a brief course of acupuncture for posttraumatic stress disorder
Engel CC, Cordova EH, Benedek DM, Liu X, Gore KL, Goertz C, et al.
Executive Summary
Write an executive summary in the form of a blog article on the topic of "Research into Chinese medicine treatment for Chronic Pain" summarising the research below and using language that can be easily understood by patients and avoiding medical jargon using a professional and caring tone of voice.
Write an executive summary in the form of a blog article on the topic of "Researched Chinese medicine treatments for Chronic Pain" summarising the research below in an objective and easy to understand way, and using language that can be easily understood by patients. Group the article into Chinese medicine treatments first, followed by nutrition and other treatments. Avoid using medical jargon and use a professional and caring tone of voice.
Write me a concise but easy to understand executive summary on the topic of "Chinese medicine treatments for Chronic Pain" based on the following research that I will give you. Your summary should be 2 paragraphs long in Australian English spelling and include references to the studies.
A Review Article published in 2022 in the journal Expert Review of Neurotherapeutics found that A 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important. The study began by revisiting previous research on acupuncture as a treatment for headache, finding shortcomings in many of these studies. It explored the influence of acupuncture on migraine and how it potentially functions. The methodology involved running several large, randomized trials comparing the use of acupuncture to conventional prophylactic drug treatments, spanning a time frame of six weeks to six months, respectively.
In the discussion of the results, it was found that the 6-week acupuncture treatment was just as effective in treating migraines as the 6-month drug treatment. Specific attributes of the acupuncture treatment, such as the selection and stimulation of Chinese points and the depth of the needles, were found to have lower significance than traditionally believed. The paper therefore suggested the integration of acupuncture into existing migraine therapy protocols.
A Systematic Review published in 2022 in the journal International Journal of Environmental Research and Public Health found that Dietary strategies, such as caloric restriction and ketogenic diets, can alleviate chronic pain and enhance quality of life. This systematic review selected 16 articles from various databases including PubMed, Web of Sciences, ProQuest, and Scopus that were published within the last 6 years. These consisted of randomized clinical trials (RCTs), observational studies, and systematic reviews evaluating the effectiveness of different dietary strategies in the treatment of chronic pain. A range of assessment scales—PEDro, PVI, QUALSYT and the Quality Assessment Tool of Systematic Reviews scale— were utilized to gauge the risk of bias in these studies.
The findings indicate an inconclusive consensus on the impact of an intermittent fasting (IF) diet on pain improvement. However, a caloric restriction diet emerged as a potential long-term treatment option for pain. Additionally, time-restricted food and ketogenic diets showed promising results in improving life quality in chronic conditions. Despite some studies indicating opposite results, the majority of the selected articles exhibited good methodological quality on their respective assessment scales.
A Systematic Review published in 2022 in the journal BioMed Research International found that Acupuncture can reduce pain and improve functional activities in patients with knee osteoarthritis, proving particularly beneficial for chronic sufferers and enhancing their quality of life. This study amassed randomized controlled trials from various databases including PubMed, Embase, and others to assess the effectiveness of acupuncture in alleviating the symptoms of knee osteoarthritis. The researchers conducted a meta-analysis using the Cochrane systematic review method by integrating Review Manager 5.4 and TSA 0.9.5.10 beta software, in conjunction with the GRADE approach for quality assessment of the evidence. They also implemented a trial sequential analysis to manage random errors and calculate the required information size.
The meta-analysis included eleven randomized controlled trials involving 2484 patients. The results indicate a positive effect of acupuncture on reducing pain and enhancing patient functionality. Conversely, stiffness symptoms were not significantly alleviated by acupuncture. Moreover, the analysis demonstrated no substantial difference between the effectiveness of acupuncture and sham procedures in improving the psychological aspects of patients' quality of life. Furthermore, physical health improvement, as measured by SF-36 or SF-12, was not significantly different between groups receiving real or sham acupuncture. The trial sequential analysis graphs showed cumulative Z-curves crossing the traditional statistical level favoring acupuncture, highlighting its potential usefulness. Therefore, acupuncture shows promise as an alternative therapy for patients with knee osteoarthritis.
A Network Pharmacology published in 2022 in the journal Annals of Medicine found that The Gui Zhi-Shao Yao herb pair in traditional Chinese medicine potentially treats chronic pain, anxiety, and depression through interactions with nine key targets. The methodology in this research utilised network pharmacology to explore the active components of the "Gui Zhi-Shao Yao" herb pair and their possible targets. Initially, 15 active compounds were identified through a series of analysis which revealed about 130 potential targets. By considering the intersections between the targets of the "Gui Zhi-Shao Yao" herb pair and chronic pain, anxiety disorder, and mental depression, nine vital targets were identified and listed in order of importance.
The results discussion revealed that the "Gui Zhi-Shao Yao" herb pairing acted on the nine identified key targets to alleviate chronic pain, anxiety, and depression. Gene ontology and pathway analysis demonstrated that there were 11 primary pathways, including AGE-RAGE signalling pathway, IL-17 signalling pathway, and TNF signalling pathway. These pathways appear to be actively involved in the pathological processes, providing a holistic understanding of how the "Gui Zhi-Shao Yao" herb pair functions therapeutically.
A Systematic Review published in 2021 in the journal Journal of Clinical Pharmacy and Therapeutics found that Acupuncture appears to have an effect on diabetic peripheral neuropathy, effectively improving nerve conduction and clinical symptoms. Acupuncture appears to have an effect on DPN, effectively improving nerve conduction and clinical symptoms. Although the methodological quality of the included studies was generally very low and defects were frequent, our study highlights areas where improvement in methodology is required. There is a need for further study of the pathogenesis of DPN, and for developing a unified standard for methods of acupuncture treatment, acupoint selection, and adverse reactions reporting. Traditional Chinese medical practices such as acupuncture should adopt an evidence-based approach to provide greater confidence in their use.
A Systematic Review published in 2020 in the journal Evidence-Based Complementary and Alternative Medicine found that In the treatment of chronic pain with depression, acupuncture could not only achieve better clinical efficacy, but also have higher safety compared with conventional mediation therapy. Acupuncture has a promising application prospect due to its unique advantages for the treatment of chronic pain with depression comorbidity, which can be used in patients suffering from some certain chronic pain with depression comorbidity with poorer response to the conventional medication or suffering from serious side effects.
A Review Article published in 2020 in the journal Phytotherapy Research found that Ginger, through various methods, exhibits promising pain reduction effects for conditions such as dysmenorrhea, muscle soreness, osteoarthritis, low back pain, and migraines. The review incorporates a vast range of randomized controlled trials conducted over the past decade, where ginger was mainly used for pain relief in distinct conditions. The conditions included dysmenorrhea, delayed onset muscle soreness, osteoarthritis, chronic low back pain, and migraines. The variety of methods used included oral administration, topical application, and aromatic oil massages.
In the analysed trials, for dysmenorrhea and muscle soreness, the considered studies suggested a promising effect after both oral and topical administration of ginger. As for osteoarthritis, most trials demonstrated pain reduction following topical and oral use of ginger, one focused on the beneficial effects of ginger in relieving migraine pain. Last but not least, a trial involving massages with aromatic ginger oil highlighted its potential in reducing chronic low back pain.
A Review Article published in 2020 in the journal Plants found that Pomegranate, due to its polyphenols, flavonoids and fatty acids, exhibits significant pain-relieving effects and could potentially be used as a treatment for various types of pain. The methodology utilized in the research consisted of conducting a review of scientific articles that met specific inclusion criteria. They focused on the use of different parts of a pomegranate and how they impact different kinds of pain. Special attention was given to the antinociceptive effect of pomegranate, with the potential mechanisms of action being closely scrutinized.
The results of the review have provided evidence that the pomegranate plant contains elements that have an antinociceptive effect and that this effect could be due to the presence of compounds like polyphenols, flavonoids, and fatty acids. The analyses suggest that these effects might be due to the activation of the L-arginine / NO pathway, TRP superfamily members (TRPA1 or TRPV1) and the opioid system. Implications for the field include understanding the mechanisms by which this effect is generated to potentially develop alternative treatments for specific types of pain, aiming to both alleviate discomfort and reduce the adverse effects produced by traditional drugs. The research proposes that the pomegranate could be further considered for the treatment of inflammatory, nociceptive, and neuropathic pain.
A Systematic Review published in 2020 in the journal Pain Research & Management found that Acupuncture reduced more headache days and the times of using painkiller and was more effective in reducing the frequency and degree of headache than western medicine and sham acupuncture. Based on high quality of evidence, we conclude that acupuncture is more effective and safer than medication or sham acupuncture in the treatment of migraine. However, the methodological quality, risk of bias, and reporting quality of SRs in acupuncture for migraine still needs improvement in future.
A Randomised Controlled Trial published in 2020 in the journal Journal of General Internal Medicine found that Both individual and group acupuncture therapy delivered in primary care settings reduced chronic pain and improved physical function at 12 weeks. Our results demonstrate that individual and group acupuncture can be offered safely in the community health center setting, that acceptability to patients and clinicians is very high, and that a substantial proportion of patients with chronic pain will have clinically significant improvement in both pain and overall physical health. Based on these results, acupuncture therapy should be offered as part of pain care to underserved populations in the primary care setting. Non-inferiority of group treatment was not demonstrated, suggesting that further research is needed on the optimal strategy for delivering group acupuncture in this context to consider it as effective as individual treatment.
A Systematic Review published in 2019 in the journal Headache found that There is growing evidence that acupuncture is just as effective and has fewer side effects than many of the standard pharmaceutical agents that are currently used. Out of the 706 search results, 7 clinical trials, with a total of 1430 participants, met inclusion criteria for trials comparing the effectiveness of acupuncture to standard pharmacologic treatment. Several of the studies showed acupuncture to be more effective than standard pharmacological treatments for migraine prevention; however, methodological heterogeneity precluded aggregation of these data.
A Review Article published in 2019 in the journal Neuropediatrics found that Currently, acupuncture is considered to be a safe, helpful, and available alternative option for patients who have not responded to or complied with conventional pharmacotherapy. The authors conducted an exhaustive review of existing literature exploring the use of acupuncture to address migraine headaches in children. This review encompassed understanding the neurobiological mechanisms of acupuncture, studies on adult headaches, pediatric headache studies, consideration of acupuncture's safety, and its application in other health conditions present in children.
The findings of this review suggested that acupuncture emerges as a safe and effective treatment option for migraine in children. Evidence proposes that it can be effectively integrated into the primary treatment regime to reduce the child's discomfort and pain. The effectiveness of acupuncture comes with the added advantage of being safe, with negligible risks, especially important when dealing with young patients. These insights support acupuncture to be seriously considered as an auxiliary treatment strategy for migraines in children.
A Systematic Review published in 2019 in the journal Evidence-Based Complementary and Alternative Medicine found that Acupuncture therapy is an effective and safe treatment for chronic pain-related insomnia. In our current study, we pooled the data from nine studies involving 944 patients. Our pooled analysis indicated that acupuncture treatment was significantly better than drugs group in improving effective rate and cure rate and in debasing PSQI score and VAS score. In addition, compared with sham acupuncture, manual acupuncture treatment has an advantage in improving the effective rate and reducing the PSQI score, but the two groups have no statistical significance in improving the cure rate. In this meta-analysis, only four studies reported relevant adverse events. The combined data showed no significant difference in adverse reactions between acupuncture group and control group. Therefore, we can carefully recommend that acupuncture is as safe as control group for CPRI. In addition, adverse events were relatively mild, mainly including bruises, soreness, nausea, dizziness, and other discomforts. These adverse events can be effectively avoided by strengthening the aseptic operation specification, and improving the professional ability of doctors. Based on the findings of our included studies, we propose that acupuncture is an effective and safe therapy for patients with CPRI.
A Randomised Controlled Trial published in 2019 in the journal Arthritis Research & Therapy found that Strong electroacupuncture for at least two weeks improves chronic pain management in knee osteoarthritis patients better than weak or sham electroacupuncture. In this investigation, a multicenter, three-arm parallel, single-blind randomized controlled trial was conducted in which 301 patients suffering from knee osteoarthritis were randomly divided into three groups based on the electroacupuncture current intensity: strong, weak, and sham. Treatments were carried out in five sessions per week over a two-week period. The impact of these treatments was primarily measured by assessing the Visual Analog Scale, conditioned pain modulation function, and the Western Ontario and McMaster Universities Osteoarthritis Index.
After a week of electroacupuncture, a clinically significant improvement was observed in Visual Analog Scale scores and Western Ontario and McMaster Universities Osteoarthritis Index scores, but not in conditioned pain modulation function. However, after two weeks of treatment, improvements were seen in all three primary outcomes when compared to baseline. In terms of enhancing conditioned pain modulation function specifically, both weak and strong electroacupuncture outperformed the sham option, with strong electroacupuncture showing superiority to weak, and resulted in better pain management.
A Systematic Review published in 2019 in the journal Acupuncture in Medicine found that Acupuncture, regardless of the trial design, showed a positive effect on pain-related outcome measures for participants with diabetic peripheral neuropathy. Acupuncture, regardless of the trial design, showed a positive effect on pain-related outcome measures for participants with DPN. However, a meta-analysis could not be performed owing to the highly heterogeneous outcome measures and limited number of high-quality RCTs available. Findings from this review showed that acupuncture improves symptoms despite the variations in acupuncture dosage, and provides beneficial effects in comparison with vitamin B therapies and no treatment. However, owing to problems with control group suitability and blinding, strong non-specific effects cannot be ruled out.
A Systematic Review published in 2019 in the journal Evidence-Based Complementary and Alternative Medicine found that We found good evidence that receiving acupuncture for chronic pain is better than not receiving treatment or being placed on a waiting list and reasonable evidence that it is better than conventional or usual care. In general, our analysis demonstrated good evidence that receiving acupuncture is better than not receiving treatment or being put on a waiting list in terms of pain control. When it was compared to conventional or usual care, acupuncture presented slightly (reasonable) better outcomes. Limited evidence was found in placebo treatments that involve the expectation of needling (real or fake). However, conclusions about the effectiveness of acupuncture in treating chronic pain are still limited due to the low quality of the studies published.
A Case Report published in 2018 in the journal Acupuncture in Medicine found that Acupuncture for cluster headache may be more effective if treated in the same way as has been shown effective for trigeminal neuralgia. Acupuncture has not generally been successful for cluster headache. This may be due to acupuncturists approaching the problem as one of severe migraine. In fact, cluster headache is classed as a trigeminal autonomic cephalgia.
In this case report, episodic cluster headache is treated in the same way as has been shown effective for trigeminal neuralgia. Acupuncture is applied to the contralateral side at points appropriate for stimulating branches of the trigeminal nerve. Thus, ST2 is used for the infraorbital nerve, BL2 and Yuyao for the supratrochlear and supraorbital nerves, and Taiyang for the temporal branch of the zygomatic nerve.
A Systematic Review published in 2018 in the journal Evidence-Based Complementary and Alternative Medicine found that There is potential of acupuncture combined with conventional treatment for treating female chronic pelvic pain. This review suggests the potential of acupuncture combined with conventional treatment compared to conventional treatment alone for treating female chronic pelvic pain. However, there is insufficient evidence to conclude that acupuncture can be recommended as a complementary and alternative (CAM) treatment for women with CPP. To draw a firm conclusion, future studies should require not only lager, more rigorously designed RCTs but also research on different acupuncture treatment types.
A published in 2018 in the journal Pain Medicine found that Acupuncture therapy offered in the group setting was effective in reducing pain severity, pain interference, and depression in patients with chronic neck, back, or shoulder pain or osteoarthritis. Subjects received eight weekly acupuncture therapy sessions in a group setting. Acupuncture therapy included a combination of palpation, acupuncture needling, Tui na, Gua sha, and auricular treatment. Baseline pain levels were established in a two- to four-week run-in; assessment of the intervention impact on pain intensity, mood, and functional status were made at the end of the treatment period (eight weeks) and 16 weeks after completion of intervention (24 weeks).
Of the total 113 participants recruited for the trial, 96 completed the 24-week protocol. We found a statistically and clinically significant decrease in pain severity, pain interference, and depression in our study population. There were no serious adverse events.
Acupuncture therapy offered in the group setting was effective in reducing pain severity, pain interference, and depression in patients with chronic neck, back, or shoulder pain or osteoarthritis. Benefit persisted through the 24-week measure despite no additional treatment. This finding has potentially important implications for improving access to effective acupuncture treatment for patients with limited financial resources.
A Systematic Review published in 2018 in the journal The Journal of Alternative and Complementary Medicine found that Patients in both group and individual acupuncture study arms valued the pain relief, improved quality of life, and relaxation experienced during acupuncture. Group acupuncture can decrease cost and increase capacity by decreasing clinic space needs and increasing patient volume per acupuncturist; however, the effectiveness and patient acceptability of group and individual session acupuncture have never been directly compared.
Patients in both study arms valued the pain relief, improved quality of life, and relaxation experienced during acupuncture. Privacy and mixed-sex groups were cited as a concern by a minority of patients; however, most of those randomized to the group setting noted that these concerns abated after initiating treatment. Differences between arms included the depth of the relationship with the acupuncturist and misgivings related to the treatment space. Group dynamics varied; some groups fostered a supportive, therapeutic interaction, while others were more reserved.
A Systematic Review published in 2017 in the journal The Journal of Pain found that Acupuncture has a clinically relevant effect on chronic pain that persists over time. Referral for acupuncture treatment is a reasonable option for chronic pain patients. We included randomized trials of acupuncture needling versus either sham acupuncture or no acupuncture control for nonspecific musculoskeletal pain, osteoarthritis, chronic headache, or shoulder pain. Trials were only included if allocation concealment was unambiguously determined to be adequate. Raw data were obtained from study authors and entered into an individual patient data meta-analysis. The main outcome measures were pain and function. An additional 13 trials were identified, with data received for a total of 20,827 patients from 39 trials. Acupuncture was superior to sham as well as no acupuncture control for each pain condition (all P < .001) with differences between groups close to .5 SDs compared with no acupuncture control and close to .2 SDs compared with sham. We also found clear evidence that the effects of acupuncture persist over time with only a small decrease, approximately 15%, in treatment effect at 1 year.
Acupuncture is effective for the treatment of chronic musculoskeletal, headache, and osteoarthritis pain. Treatment effects of acupuncture persist over time and cannot be explained solely in terms of placebo effects. Referral for a course of acupuncture treatment is a reasonable option for a patient with chronic pain.
A Meta-Analysis published in 2017 in the journal Pain Physician found that The existing evidence suggests that most acupuncture therapies, including acupuncture combined with other therapies, are effective in decreasing pain and in improving physical function. Thirty-three trials with 1,692 patients were included. Patients were allocated to 22 kinds of interventions, of which dry needling and manual acupuncture was the most frequently investigated intervention. Compared with placebo-sham acupuncture, scraping combined with warming acupuncture and moxibustion was found to be more effective for decreasing pain intensity; miniscalpel-needle was more effective for increasing the PPT; trigger points injection with bupivacaine was associated with the highest risk of adverse event; and only EA showed a significant difference in the ROM.
A Systematic Review published in 2017 in the journal Pain found that Patients with chronic pain can generally be reassured that treatment effects persist after a course of treatment with acupuncture. The available individual patient data set included 29 trials and 17,922 patients. The chronic pain conditions included musculoskeletal pain (low back, neck, and shoulder), osteoarthritis of the knee, and headache/migraine. We used meta-analytic techniques to determine the trajectory of posttreatment pain scores. Data on longer term follow-up were available for 20 trials, including 6376 patients. In trials comparing acupuncture to no acupuncture control (wait-list, usual care, etc), effect sizes diminished by a nonsignificant 0.011 SD per 3 months after treatment ended. The central estimate suggests that approximately 90% of the benefit of acupuncture relative to controls would be sustained at 12 months. For trials comparing acupuncture to sham, we observed a reduction in effect size of 0.025 SD per 3 months, suggesting approximately a 50% diminution at 12 months.
The effects of a course of acupuncture treatment for patients with chronic pain do not seem to decrease importantly over 12 months. Patients can generally be reassured that treatment effects persist. Studies of the cost-effectiveness of acupuncture should take our findings into account when considering the time horizon of acupuncture effects. Further research should measure longer term outcomes of acupuncture.
A Systematic Review published in 2017 in the journal Programme Grants for Applied Research found that The programme of research found that acupuncture was more effective than usual care and sham acupuncture for chronic pain, that it was one of the more clinically effective physical therapies for osteoarthritis and that it showed benefits in the treatment of depression. We have provided the most robust evidence from high-quality trials on acupuncture for chronic pain. The synthesis of high-quality IPD found that acupuncture was more effective than both usual care and sham acupuncture. Acupuncture is one of the more clinically effective physical therapies for osteoarthritis and is also cost-effective if only high-quality trials are analysed. When all trials are analysed, TENS is cost-effective. Promising clinical and economic evidence on acupuncture for depression needs to be extended to other contexts and settings. For the conditions we have investigated, the drawing together of evidence on acupuncture from this programme of research has substantially reduced levels of uncertainty. We have identified directions for further research. Our research also provides a valuable basis for considering the potential role of acupuncture as a referral option in health care and enabling providers and policy-makers to make decisions based on robust sources of evidence.
A Randomised Controlled Trial published in 2016 in the journal Neural Regeneration Research found that A 14-session course of needling at Fengchi is relatively safe for treating posterior circulation ischemia with vertigo. Acupuncture at Fengchi (GB20) in the posterior neck improves vertigo. However, subarachnoid hemorrhage and spinal epidural hematoma have been reported to occur after acupuncture in the posterior neck. Therefore, in the present study, we assessed the safety of acupuncture at Fengchi.
Of the 136 patients, 120 completed the study. There were no significant differences between pretreatment and posttreatment test results in any of the groups. Only five patients suffered from minor adverse events (needling pain, slight hematoma and transient chest tightness). No serious adverse events were found. Our results indicate that a 14-session course of needling at Fengchi is relatively safe for treating posterior circulation ischemia with vertigo.
A Systematic Review published in 2016 in the journal Scientific Reports found that Clinicians may consider Tai Chi as a viable complementary and alternative medicine for chronic pain conditions. The aggregated results have indicated that Tai Chi showed positive evidence on immediate relief of chronic pain from osteoarthritis. The valid duration of Tai Chi practice for osteoarthritis may be more than 5 weeks. And there were some beneficial evidences regarding the effects of Tai Chi on immediate relief of chronic pain from low back pain and osteoporosis. Therefore, clinicians may consider Tai Chi as a viable complementary and alternative medicine for chronic pain conditions.
A Systematic Review published in 2015 in the journal Neurology found that The majority of trials demonstrate a positive effect of acupuncture over control condition in the treatment of neuropathy. The majority of RCTs reviewed showed clear benefit for acupuncture over control in the treatment of diabetic neuropathy, Bell’s palsy and carpal tunnel syndrome. Acupuncture is probably effective in the treatment of HIV-related neuropathy and there is insufficient evidence for its benefits in idiopathic neuropathy. Meta-analyses of all diabetic neuropathy and bell’s palsy data using a summary estimate random effects model showed combined Odds Ratio (OR) of 4.23, p<0.001 favoring acupuncture over control for pain outcomes. The majority of trials demonstrate a positive effect of acupuncture over control condition in the treatment of neuropathy. Further more rigorously designed studies are needed to better characterize this effect.
A Randomised Controlled Trial published in 2014 in the journal Medical Care found that Improvement in post traumatic stress disorder severity was significantly greater among those receiving acupuncture than in those receiving usual PTSD care. Mean improvement in PTSD severity was significantly greater among those receiving acupuncture than in those receiving usual PTSD care (PCLΔ=19.8±13.3 vs. 9.7±12.9, P<0.001; CAPSΔ=35.0±20.26 vs. 10.9±20.8, P<0.0001). Acupuncture was also associated with significantly greater improvements in depression, pain, and physical and mental health functioning. Pre-post effect-sizes for these outcomes were large and robust.
Acupuncture was effective for reducing PTSD symptoms. Limitations included small sample size and inability to parse specific treatment mechanisms. Larger multisite trials with longer follow-up, comparisons to standard PTSD treatments, and assessments of treatment acceptability are needed. Acupuncture is a novel therapeutic option that may help to improve population reach of PTSD treatment.