Migraine
How to submit an article:
- Registered users can submit any published journal article that has a unique DOI (Digital Object Identifier) name or link to Research Hub.
- For example, you can paste the full DOI link:
https://doi.org/10.1109/5.771073or just the DOI name:10.1109/5.771073into the field above and click submit. - The person who is first to submit a valid article to Research Hub will forever be credited for it, and every article submission earns you +6 Research Points.
Published research studies are articles that present the findings of original research that has undergone a peer-review process and has been made publicly available in scholarly journals, books or other media.

Role of acupuncture in the treatment of migraine
2022 Sep Expert Review of Neurotherapeutics Endres HG, Diener HC, Molsberger A
Review Article Migraine Headache & MigraineA 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important.

Traditional Acupuncture in Migraine: A Controlled, Randomized Study
2022 Sep 14 Pain Medicine Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, et al.
Randomised Controlled TrialTrue acupuncture treatment according to traditional Chinese medicine consistently improved migraine outcomes more than just medication or mock treatments.

Functional connectivity changes during migraine treatment with electroacupuncture at Shuaigu (GB8)
2022 May Journal of Integrative Medicine Wei X, Luo S, Chen H, Liu S, Gong Z, Zhan S
The alteration of FC between the right insula subregions and multiple brain regions may be an important index for MWoA. EA at GB8 was able to adjust the FC between the right insula subregions and parietal lobe, namely, the right dAI and right postcentral gyrus, and the right PI and left precuneus, thereby rendering an instant effect in the management of MWoA.
Clinical Study Migraine
Wen Dan Tang: A Potential Jing Fang Decoction for Headache Disorders?
2022 Mar 04 Medicines Pradhan SK, Li Y, Gantenbein AR, Angst F, Lehmann S, Shaban H
Systematic Review Wen Dan TangWen Dan Tang potentially treats neurological, psychiatric disorders, cardiovascular diseases, and digestive disorders, and might improve life quality in headache patients.
Regulatory Effects of Acupuncture on Emotional Disorders in Patients With Menstrual Migraine Without Aura: A Resting-State fMRI Study
2021 Oct 04 Frontiers in Neuroscience Yutong Zhang, Ziwen Wang, Jiarong Du, Jixin Liu, Tao Xu, Xiao Wang, et al.
True acupuncture (TA) had a relatively better effect in reducing the frequency of migraine attack than sham acupuncture (SA). The two therapies have different modulation effects as TA regulates emotional disorders by modulating the frontal-limbic regions, and SA may modulate pain perception through the placebo effect on insula and by indirectly regulating emotional disorders.
Randomised Controlled Trial AcupunctureResearch insights are moderated by the Research Hub team and offer an at-a-glance overview of interesting research findings.

2022 Pain Medicine
True acupuncture treatment according to traditional Chinese medicine consistently improved migraine outcomes more than just medication or mock treatments.
Randomised Controlled Trial
Traditional Acupuncture in Migraine: A Controlled, Randomized Study
Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, et al.

2022 Expert Review of Neurotherapeutics
A 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important.
Review Article Headache & Migraine
Role of acupuncture in the treatment of migraine
Endres HG, Diener HC, Molsberger A
2022 Medicines
Wen Dan Tang potentially treats neurological, psychiatric disorders, cardiovascular diseases, and digestive disorders, and might improve life quality in headache patients.
Systematic Review Wen Dan Tang
Wen Dan Tang: A Potential Jing Fang Decoction for Headache Disorders?
Pradhan SK, Li Y, Gantenbein AR, Angst F, Lehmann S, Shaban H
2021 Evidence-Based Complementary and Alternative Medicine
Cupping therapy has beneficial therapeutic effects and could be effective for the treatment of migraine.
Systematic Review
Cupping Therapy for Migraine: A PRISMA-Compliant Systematic Review and Meta-Analysis of Randomized Controlled Trials
Jihye Seo, Hongmin Chu, Cheol-Hyun Kim, Kang-Keyng Sung, Sangkwan Lee
2021 Frontiers in Neurology
Acupuncture could be as effective as pharmacological drugs for migraine prevention, with improved patient compliance and fewer adverse events.
Randomised Controlled Trial
A Randomized Clinical Trial on Acupuncture Versus Best Medical Therapy in Episodic Migraine Prophylaxis: The ACUMIGRAN Study
Giannini G, Favoni V, Merli E, Nicodemo M, Torelli P, Matrà A, et al.
Review Articles
Review articles summarise and critically evaluate the current state of research on a specific topic or field by synthesising multiple primary research studies.

Role of acupuncture in the treatment of migraine
2022 Sep Expert Review of Neurotherapeutics Endres HG, Diener HC, Molsberger A
Review Article Migraine Headache & MigraineA 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important.
Wen Dan Tang: A Potential Jing Fang Decoction for Headache Disorders?
2022 Mar 04 Medicines Pradhan SK, Li Y, Gantenbein AR, Angst F, Lehmann S, Shaban H
Systematic Review Wen Dan TangWen Dan Tang potentially treats neurological, psychiatric disorders, cardiovascular diseases, and digestive disorders, and might improve life quality in headache patients.
Revealing the Neural Mechanism Underlying the Effects of Acupuncture on Migraine: A Systematic Review
2021 May 20 Frontiers in Neuroscience Liu L, Tian T, Li X, Wang Y, Xu T, Ni X, et al.
The neural mechanism underlying the immediate effect of acupuncture analgesia remains unclear, and the neural mechanism of sustained acupuncture treatment for migraine might be related to the regulation of pain-related brain networks. Multi-center neuroimaging studies are needed to provide a better insight into the neural mechanism underlying the effect of acupuncture on migraine.
Systematic Review Migraine
Cupping Therapy for Migraine: A PRISMA-Compliant Systematic Review and Meta-Analysis of Randomized Controlled Trials
2021 Mar 25 Evidence-Based Complementary and Alternative Medicine Jihye Seo, Hongmin Chu, Cheol-Hyun Kim, Kang-Keyng Sung, Sangkwan Lee
Systematic Review Meta-AnalysisCupping therapy has beneficial therapeutic effects and could be effective for the treatment of migraine.
Oral Chinese Herbal Medicine as Prophylactic Treatment for Episodic Migraine in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
2020 Dec 28 Evidence-Based Complementary and Alternative Medicine Lyu S, Zhang CS, Guo X, Zhang AL, Sun J, Lu C, et al.
Systematic Review Meta-AnalysisChinese herbal medicine seems to be as effective as flunarizine in reducing the frequency of migraines in adults.
Clinical Trials
Clinical trials are research studies that involve people and are conducted to evaluate the safety and efficacy of new treatments or interventions, such as drugs, medical devices, or behavioural therapies.

Traditional Acupuncture in Migraine: A Controlled, Randomized Study
2022 Sep 14 Pain Medicine Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, et al.
Randomised Controlled TrialTrue acupuncture treatment according to traditional Chinese medicine consistently improved migraine outcomes more than just medication or mock treatments.
Regulatory Effects of Acupuncture on Emotional Disorders in Patients With Menstrual Migraine Without Aura: A Resting-State fMRI Study
2021 Oct 04 Frontiers in Neuroscience Yutong Zhang, Ziwen Wang, Jiarong Du, Jixin Liu, Tao Xu, Xiao Wang, et al.
True acupuncture (TA) had a relatively better effect in reducing the frequency of migraine attack than sham acupuncture (SA). The two therapies have different modulation effects as TA regulates emotional disorders by modulating the frontal-limbic regions, and SA may modulate pain perception through the placebo effect on insula and by indirectly regulating emotional disorders.
Randomised Controlled Trial Acupuncture
A Randomized Clinical Trial on Acupuncture Versus Best Medical Therapy in Episodic Migraine Prophylaxis: The ACUMIGRAN Study
2021 Jan 15 Frontiers in Neurology Giannini G, Favoni V, Merli E, Nicodemo M, Torelli P, Matrà A, et al.
Randomised Controlled Trial MigraineAcupuncture could be as effective as pharmacological drugs for migraine prevention, with improved patient compliance and fewer adverse events.
Effectiveness of Acupuncture as Auxiliary Treatment for Chronic Headache
2018 Oct Journal of Acupuncture and Meridian Studies Mayrink WC, Garcia JBS, Dos Santos AM, Nunes JKVRS, Mendonça THN
This study showcase the effectiveness of acupuncture with chronic headache patients. The participants were found to have decreased in pain, reduced the amount of migraines attacks, reduced the amount of analgesics used, and improved the quality of life. Patients reported to have an overall better mental and physical health after treatments.
Practice Guideline Randomised Controlled Trial
The Long-term Effect of Acupuncture for Migraine Prophylaxis A Randomized Clinical Trial
2017 Apr JAMA Internal Medicine Zhao L, Chen J, Li Y, et al
This study showed that acupuncture was more efficacious for migraine patients (without aura) in the long run for at least 24 weeks. Patients reported to have reduced intake of medication (such as ibuprofen) and have less associated pain or side effects. They also have significant improvement with overall quality of life.
Randomised Controlled TrialStudy Protocols
Published study protocols are detailed plans that outline the objectives, methodology, statistical analyses, and organisation of a research study that have been made publicly available for others to review and use as a reference.
Presentation Slides

Randomised Controlled Trial
True acupuncture treatment according to traditional Chinese medicine consistently improved migraine outcomes more than just medication or mock treatments.
Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, Mattia C

Review Article
A 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important.
Endres HG, Diener HC, Molsberger A
Systematic Review
Wen Dan Tang potentially treats neurological, psychiatric disorders, cardiovascular diseases, and digestive disorders, and might improve life quality in headache patients.
Pradhan SK, Li Y, Gantenbein AR, Angst F, Lehmann S, Shaban H
Systematic Review
Cupping therapy has beneficial therapeutic effects and could be effective for the treatment of migraine.
Jihye Seo, Hongmin Chu, Cheol-Hyun Kim, Kang-Keyng Sung, Sangkwan Lee
Randomised Controlled Trial
Acupuncture could be as effective as pharmacological drugs for migraine prevention, with improved patient compliance and fewer adverse events.
Giannini G, Favoni V, Merli E, Nicodemo M, Torelli P, Matrà A, Giovanardi CM, Cortelli P, Pierangeli G, Cevoli S
Systematic Review
Chinese herbal medicine seems to be as effective as flunarizine in reducing the frequency of migraines in adults.
Lyu S, Zhang CS, Guo X, Zhang AL, Sun J, Lu C, Xue CC, Luo X
Systematic Review
Based on moderate certainty of evidence, we conclude that acupuncture is mildly more effective and much safer than medication for the prophylaxis of migraine.
Giovanardi CM, Cinquini M, Aguggia M, Allais G, Campesato M, Cevoli S, Gentili F, Matrà A and Minozzi S

Systematic Review
In many studies, acupuncture has been shown to be a safe, efficacious and readily available alternative therapy which may be beneficial to certain migraine patients.
Urits I, Patel M, Putz ME, Monteferrante NR, Nguyen D, An D, Cornett EM, Hasoon J, Kaye AD, Viswanath O.
Systematic Review
Compared with the sham acupuncture group, the acupuncture group had greater improvements in the frequency of migraine attacks, VAS score, and treatment efficiency.
Ou MQ, Fan WH, Sun FR, Jie WX, Lin MJ, Cai YJ, Liang SY, Yu YS, Li MH, Cui LL, Zhou HH

Review Article
Ginger, through various methods, exhibits promising pain reduction effects for conditions such as dysmenorrhea, muscle soreness, osteoarthritis, low back pain, and migraines.
Rondanelli M, Fossari F, Vecchio V, Gasparri C, Peroni G, Spadaccini D, Riva A, Petrangolini G, Iannello G, Nichetti M, Infantino V, Perna S

Systematic Review
Acupuncture reduced more headache days and the times of using painkiller and was more effective in reducing the frequency and degree of headache than western medicine and sham acupuncture.
Li YX, Xiao XL, Zhong DL, Luo LJ, Yang H, Zhou J, He MX, Shi LH, Li J, Zheng H, Jin RJ

Systematic Review
There is growing evidence that acupuncture is just as effective and has fewer side effects than many of the standard pharmaceutical agents that are currently used.
Niushen Zhang, Tim Houle, Nada Hindiyeh, & Sheena K. Aurora

Systematic Review
Acupuncture has the advantage for acute and preventive treatment of migraine in pain improvement and safety.
Xia-tian Zhang, Xin-yi Li, Chen Zhao, Ye-yin Hu, Yi-yi Lin, He-qing Chen, Zhao-feng Shi, Xiao-yu Zhang, Hong-cai Shang, Gui-hua Tian

Review Article
Currently, acupuncture is considered to be a safe, helpful, and available alternative option for patients who have not responded to or complied with conventional pharmacotherapy.
Doll, E., Threlkeld, B., Graff, D., Clemons, R., Mittel, O., Sowell, M. K.
Systematic Review
The results of this meta-analysis showed that acupuncture is more effective and safer than medication for migraine.
SHEN, Feng-jiao AU - XU, Jia AU - ZHAN, Yi-jun AU - FU, Qin-hui AU - PEI, Jian PY
Systematic Review
The available evidence suggests that adding acupuncture to symptomatic treatment of attacks reduces the frequency of headaches.
Linde K, Allais G, Brinkhaus B, et al.
Clinical Study
Migraine patients exhibit lower intracellular magnesium levels, which can be increased by consuming magnesium-rich mineral water, demonstrating its bioavailability.
Thomas J, Millot JM, Sebille S, Delabroise AM, Thomas E, Manfait M, Arnaud MJ
Executive Summary
Write an executive summary in the form of a blog article on the topic of "Research into Chinese medicine treatment for Migraine" summarising the research below and using language that can be easily understood by patients and avoiding medical jargon using a professional and caring tone of voice.
Write an executive summary in the form of a blog article on the topic of "Researched Chinese medicine treatments for Migraine" summarising the research below in an objective and easy to understand way, and using language that can be easily understood by patients. Group the article into Chinese medicine treatments first, followed by nutrition and other treatments. Avoid using medical jargon and use a professional and caring tone of voice.
Write me a concise but easy to understand executive summary on the topic of "Chinese medicine treatments for Migraine" based on the following research that I will give you. Your summary should be 2 paragraphs long in Australian English spelling and include references to the studies.
A Randomised Controlled Trial published in 2022 in the journal Pain Medicine found that True acupuncture treatment according to traditional Chinese medicine consistently improved migraine outcomes more than just medication or mock treatments. In the prospective, randomized, controlled study, 160 migraine patients without aura were assigned to one of four treatment groups. These treatments included: traditional Chinese medicine acupuncture combined with Rizatriptan (TA); a ritualized non-penetrative acupuncture treatment combined with Rizatriptan (RMA); a standard non-penetrative acupuncture treatment combined with Rizatriptan (SMA); or Rizatriptan alone (R). The Migraine Disability Assessment (MIDAS) questionnaire was completed before treatment, and again after three and six months. The study found that all patient groups experienced a decrease in Migraine Disability Assessment scores following treatment, indicating general improvement. However, the traditional acupuncture treatment group (TA) showed significant improvement in comparison to those who received only Rizatriptan. The ritualized non-penetrative acupuncture treatment group (RMA) showed temporary improvement, suggesting a placebo effect.
A Review Article published in 2022 in the journal Expert Review of Neurotherapeutics found that A 6-week course of acupuncture proves as effective as 6-month drug prophylaxis for migraines, with specific Chinese point selection and stimulation appearing less important. The study began by revisiting previous research on acupuncture as a treatment for headache, finding shortcomings in many of these studies. It explored the influence of acupuncture on migraine and how it potentially functions. The methodology involved running several large, randomized trials comparing the use of acupuncture to conventional prophylactic drug treatments, spanning a time frame of six weeks to six months, respectively. In the discussion of the results, it was found that the 6-week acupuncture treatment was just as effective in treating migraines as the 6-month drug treatment. Specific attributes of the acupuncture treatment, such as the selection and stimulation of Chinese points and the depth of the needles, were found to have lower significance than traditionally believed. The paper therefore suggested the integration of acupuncture into existing migraine therapy protocols.
A Systematic Review published in 2022 in the journal Medicines found that Wen Dan Tang potentially treats neurological, psychiatric disorders, cardiovascular diseases, and digestive disorders, and might improve life quality in headache patients. The methodology of the study included the utilization of various online databases like PubMed, Medline, Cochrane Library, AcuTrials, Embase, Semantic Scholar, Jstor, and internet research. The study also involved reviewing ancient and modern Chinese medical textbooks. The research noted that while there were no dedicated studies on Wen Dan Tang in the context of migraine and tension-type headaches, it gathered and examined data for each compound found in the formula. The discussion of the results revealed the therapeutic potential of the bioactive compounds present in Wen Dan Tang. This was especially in the case of patients with neurological and psychiatric disorders, cardiovascular diseases, metabolic syndrome, and digestive disorders. Additionally, the correlations between Wen Dan Tang and the reduction of headaches were explored. A potential improvement in the quality of life was highlighted, especially for patients suffering from migraines and tension-type headaches.
A Systematic Review published in 2021 in the journal Evidence-Based Complementary and Alternative Medicine found that Cupping therapy has beneficial therapeutic effects and could be effective for the treatment of migraine. We analyzed 6 RCTs with 510 migraine participants in this review and the results show that wet cupping and dry cupping could improve the migraine symptoms. No significant adverse events were identified in the studies included in this review. This review is the first comprehensive systematic review and meta-analysis about cupping therapy for migraine. In addition, the levels of evidence were presented through assessment of the quality of the evidence. The quality of the level of evidence was low in the wet cupping versus drugs group and dry cupping plus acupuncture versus acupuncture group. Regardless of the potential bias and limitations, all the included studies concluded that cupping therapy had beneficial therapeutic effects in treating migraine. Cupping therapy has potential therapeutic effects on treating migraine. Further larger and rigorously designed RCTs are needed to confirm the cupping therapy’s therapeutic effect. Additional economic studies might be considered for future studies to compare the cost-effectiveness of cupping therapy plus acupuncture or cupping therapy plus drugs.
A Randomised Controlled Trial published in 2021 in the journal Frontiers in Neurology found that Acupuncture could be as effective as pharmacological drugs for migraine prevention, with improved patient compliance and fewer adverse events. In the study, patients experiencing migraines who hadn't undergone preventive treatment in the prior 3 months were randomly divided into two groups. Group A underwent 12 acupuncture sessions, while Group B received a range of suitable medications for each individual. The frequency of headaches was compared at the beginning and end of treatment, and both groups were assessed after three and six months post-treatment. Results highlighted that both treatments led to a significant decrease in headache frequency. Of the patients, around 34% saw a 50% reduction of headache days post-treatment. The improvements seen at the end of treatment were maintained in 57.3% of patients three months after and in 38.8% of patients six months after, notably in the acupuncture group. Based on this data, acupuncture can be seen as an effective alternative for migraine prophylaxis.
A Systematic Review published in 2020 in the journal Evidence-Based Complementary and Alternative Medicine found that Chinese herbal medicine seems to be as effective as flunarizine in reducing the frequency of migraines in adults. The study involved a comprehensive search across nine databases, looking for randomized controlled trials focusing on the application of Chinese herbal medicine in treating episodic migraines as compared to flunarizine. After filtering out non-relevant trials, thirty-five studies with a total of 2,840 participants were chosen, and 31 of them were further assessed in meta-analyses. The treatment's effectiveness was evaluated at both the end of the treatment period and the end of the follow-up period. The study discovered that Chinese herbal medicine was effective in reducing the frequency of migraines at the end treatment and the end of follow-up. This was regardless of the duration of treatment or follow-up, and the dosage of flunarizine taken. Sub-analyses divided based on these parameters showed the Chinese herbal medicine was comparable, if not superior, to flunarizine. Similarly positive results were observed in terms of secondary goals like pain scale, migraine duration, response rate, and usage of acute medication. The studies using specific Chinese herb pairs were particularly promising.
A Systematic Review published in 2020 in the journal Frontiers in Neurology found that Based on moderate certainty of evidence, we conclude that acupuncture is mildly more effective and much safer than medication for the prophylaxis of migraine. We included in our meta-analysis 9 studies, with a total of 1,484 participants that compared acupuncture with pharmacological prophylaxis for the prevention of migraine attacks in adults with chronic or episodic migraine. We found moderate quality of evidence that acupuncture is mildly more effective than any pharmacological prophylaxis in reducing the days with migraine per month, pain intensity, drop out from treatment, though the magnitude of the differences was small. We also found moderate quality of evidence that acupuncture is more effective than pharmacological prophylaxis in increasing the response rate to treatments and quality of life, but the magnitude of the differences was small. Conversely, we found moderate quality of evidence of a strong reduction in favor of acupuncture in both the dropout rate due to any and in the dropout rate due to adverse event.
A Systematic Review published in 2020 in the journal Neurology and Therapy found that In many studies, acupuncture has been shown to be a safe, efficacious and readily available alternative therapy which may be beneficial to certain migraine patients. Migraines are difficult to treat, and current treatment options have many unwanted side effects, such as exacerbating headache pain in those with chronic migraine. Therefore, while the primary treatment for migraines is drug therapy, acupuncture is gaining increasing attention as a viable addition to the treatment management of migraine patients due to its measurable effects on both the duration and frequency of migraine attacks. Many studies suggest that acupuncture is a safe, helpful and available alternative therapy that may be beneficial to certain migraine patients. Nevertheless, further large-scale RCTs are warranted to further consolidate these findings and provide further support for the clinical value of acupuncture.
A Systematic Review published in 2020 in the journal Frontiers in Neurology found that Compared with the sham acupuncture group, the acupuncture group had greater improvements in the frequency of migraine attacks, VAS score, and treatment efficiency. Meta-analysis of 28 articles showed that acupuncture treatment has higher treatment efficiency than sham acupuncture treatment, and acupuncture can reduce the frequency of migraine attacks and ameliorate the visual analog scale (VAS) score more significantly. Compared with the medication (medication group), acupuncture treatment is more effective and the incidence of adverse reactions is lower. In addition, the transcranial doppler (TCD) analysis results suggested that the acupuncture group has a better hemodynamic improvement effect than the medication group, but the results need to be further verified due to the existence of heterogeneity.
A Review Article published in 2020 in the journal Phytotherapy Research found that Ginger, through various methods, exhibits promising pain reduction effects for conditions such as dysmenorrhea, muscle soreness, osteoarthritis, low back pain, and migraines. The review incorporates a vast range of randomized controlled trials conducted over the past decade, where ginger was mainly used for pain relief in distinct conditions. The conditions included dysmenorrhea, delayed onset muscle soreness, osteoarthritis, chronic low back pain, and migraines. The variety of methods used included oral administration, topical application, and aromatic oil massages. In the analysed trials, for dysmenorrhea and muscle soreness, the considered studies suggested a promising effect after both oral and topical administration of ginger. As for osteoarthritis, most trials demonstrated pain reduction following topical and oral use of ginger, one focused on the beneficial effects of ginger in relieving migraine pain. Last but not least, a trial involving massages with aromatic ginger oil highlighted its potential in reducing chronic low back pain.
A Systematic Review published in 2020 in the journal Pain Research & Management found that Acupuncture reduced more headache days and the times of using painkiller and was more effective in reducing the frequency and degree of headache than western medicine and sham acupuncture. Based on high quality of evidence, we conclude that acupuncture is more effective and safer than medication or sham acupuncture in the treatment of migraine. However, the methodological quality, risk of bias, and reporting quality of SRs in acupuncture for migraine still needs improvement in future.
A Systematic Review published in 2019 in the journal Headache found that There is growing evidence that acupuncture is just as effective and has fewer side effects than many of the standard pharmaceutical agents that are currently used. Out of the 706 search results, 7 clinical trials, with a total of 1430 participants, met inclusion criteria for trials comparing the effectiveness of acupuncture to standard pharmacologic treatment. Several of the studies showed acupuncture to be more effective than standard pharmacological treatments for migraine prevention; however, methodological heterogeneity precluded aggregation of these data.
A Systematic Review published in 2019 in the journal Pain Research & Management found that Acupuncture has the advantage for acute and preventive treatment of migraine in pain improvement and safety. This overview included a considerable number of systematic reviews/meta analyses (SR/MAs), illustrating that acupuncture has the advantage in pain improvement of VAS score, headache days/frequency, analgesic use and efficacy of response rate, and effective rate according to the present evidence. In terms of conclusion, the results of all 15 (100%) SR/MAs were positive. For treatment, 6 SR/MAs reported acupuncture had superiority relative to drugs; 4 SR/MAs reported acupuncture had superiority relative to sham acupuncture, drugs; 3 SR/MAs reported acupuncture had superiority relative to sham acupuncture; 1 SR/MA reported acupuncture had superiority relative to drugs, other TCM treatments. 1 SR/MA reported that acupuncture had superiority in treating migraine, but did not mention the control group in the conclusions. Based on previous evidence we reviewed, we supposed acupuncture might be a kind of available treatment for migraine in preventive or acute treatment, but in consideration of low methodological quality of present SR/MAs or RCTs of acupuncture for migraine, we need more high-quality evidence to demonstrate the effect of acupuncture for migraine.
A Review Article published in 2019 in the journal Neuropediatrics found that Currently, acupuncture is considered to be a safe, helpful, and available alternative option for patients who have not responded to or complied with conventional pharmacotherapy. The authors conducted an exhaustive review of existing literature exploring the use of acupuncture to address migraine headaches in children. This review encompassed understanding the neurobiological mechanisms of acupuncture, studies on adult headaches, pediatric headache studies, consideration of acupuncture's safety, and its application in other health conditions present in children. The findings of this review suggested that acupuncture emerges as a safe and effective treatment option for migraine in children. Evidence proposes that it can be effectively integrated into the primary treatment regime to reduce the child's discomfort and pain. The effectiveness of acupuncture comes with the added advantage of being safe, with negligible risks, especially important when dealing with young patients. These insights support acupuncture to be seriously considered as an auxiliary treatment strategy for migraines in children.
A Systematic Review published in 2019 in the journal World Journal of Acupuncture-Moxibustion found that The results of this meta-analysis showed that acupuncture is more effective and safer than medication for migraine. A total of 13 trails including 1218 participants met the selection criteria. The meta-analysis of 3 articles showed that acupuncture was more effective in reducing the frequency of migraine attacks than medication. The meta-analysis of three articles showed that acupuncture was more effective in reducing the number of migraine days than medication after treatment. The meta-analysis of six articles showed that acupuncture was more effective in reducing VAS after treatment. The meta-analysis of two articles showed that acupuncture was more effective in reducing VAS during follow-up. The meta-analysis of seven articles showed that the total effective rate of acupuncture was higher than that of medication. In addition, fewer adverse effects in acupuncture groups were reported than in medication groups. Overall the quality of the evidence was low. The results of this meta-analysis showed that acupuncture is more effective and safer than medication for migraine. Acupuncture can be considered a treatment option for patients willing to undergo this treatment. But more high-quality studies, based on standardized, comprehensive and objective evaluation, are required to enhance the reliability of the conclusion.
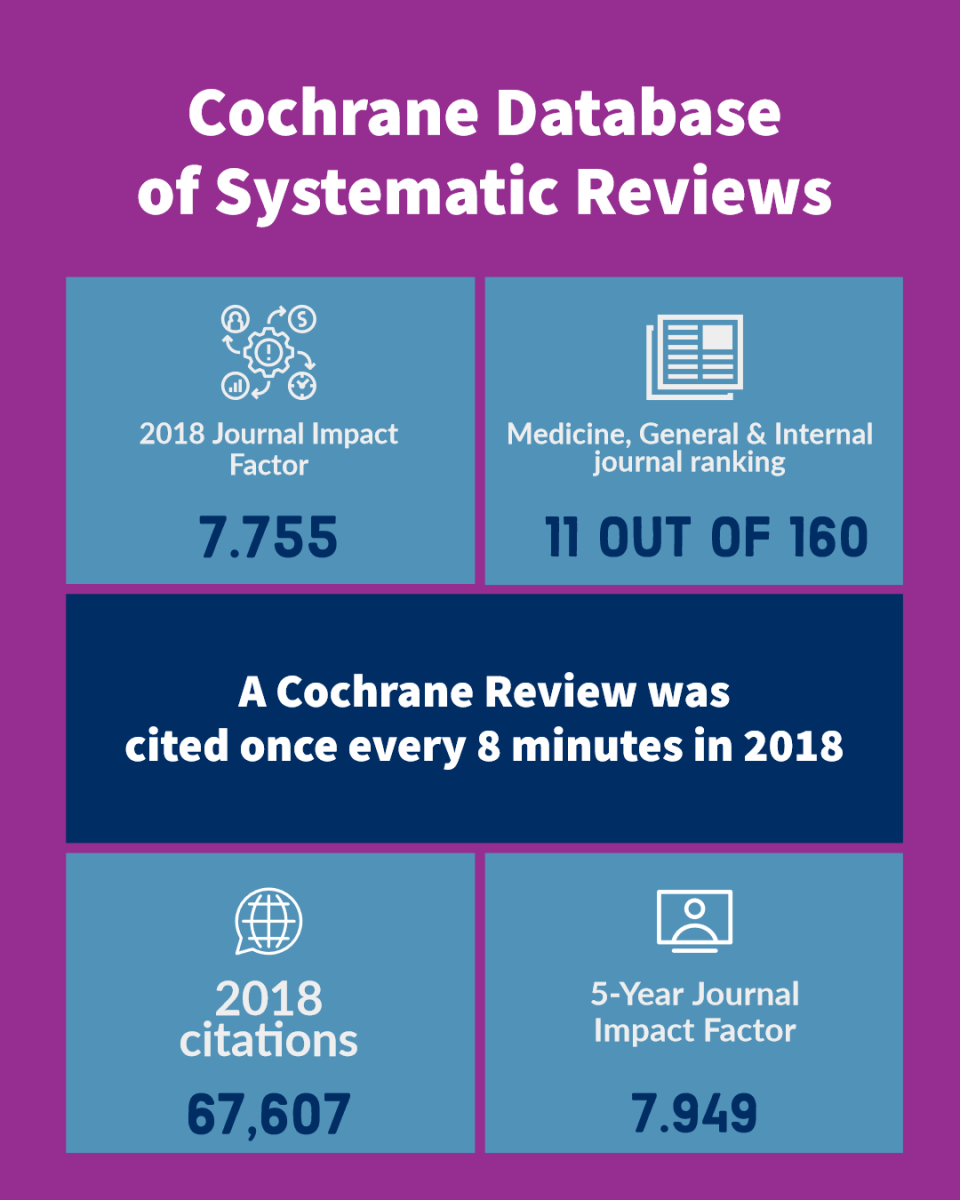
A Systematic Review published in 2016 in the journal Cochrane Database of Systematic Reviews found that The available evidence suggests that adding acupuncture to symptomatic treatment of attacks reduces the frequency of headaches. Contrary to the previous findings, the updated evidence also suggests that there is an effect over sham, but this effect is small. The available trials also suggest that acupuncture may be at least similarly effective as treatment with prophylactic drugs. Acupuncture can be considered a treatment option for patients willing to undergo this treatment.
A Clinical Study published in 2000 in the journal Clinica Chimica Acta found that Migraine patients exhibit lower intracellular magnesium levels, which can be increased by consuming magnesium-rich mineral water, demonstrating its bioavailability. The study started by identifying a common issue with lower-than-recommended dietary intakes of magnesium in Western countries. The focus was on migraine patients, as low brain magnesium and impaired magnesium metabolism had been reported in migraine cases. A non-invasive and sensitive test to detect these deficiencies was sought. Magnesium, being an intracellular cation, was tested in 29 migraine patients and 18 control subjects. The tests were for total magnesium in plasma, erythrocytes, lymphocytes and ionized magnesium in lymphocytes. The analysis found that there were lower concentrations of total magnesium in erythrocytes and ionized magnesium in lymphocytes of migraine patients compared to controls. These findings indicated a notable overall difference between the migraine patients and the controls, despite there being overlaps in some individual values. The researchers then subjected the migraine patients to a 2-week intake of a mineral water rich in magnesium. An increase in all intracellular magnesium concentrations was observed, with no effect on plasma magnesium. This increase demonstrated the bioavailability of magnesium from the mineral water. Interestingly, the most sensitive index of magnesium deficiency turned out to be ionized magnesium in lymphocytes, which saw the most significant increase after the intake of the magnesium-rich mineral water.
Moderation Tools
Topic
Sign In
Users not signed in are limited to viewing the 5 most recent items of content.