Colitis
How to submit an article:
- Registered users can submit any published journal article that has a unique DOI (Digital Object Identifier) name or link to Research Hub.
- For example, you can paste the full DOI link:
https://doi.org/10.1109/5.771073or just the DOI name:10.1109/5.771073into the field above and click submit. - The person who is first to submit a valid article to Research Hub will forever be credited for it, and every article submission earns you +6 Research Points.
Related Topics
Published research studies are articles that present the findings of original research that has undergone a peer-review process and has been made publicly available in scholarly journals, books or other media.

Lactobacillus acidophilus 6074 Fermented Jujube Juice Ameliorated DSS‐induced Colitis via Repairing Intestinal Barrier, Modulating Inflammatory Factors, and Gut Microbiota
2024 Dec 15 Molecular Nutrition & Food Research Li H, Fan L, Yang S, Tan P, Lei W, Yang H, et al.
Animal Study Lactobacillus Gut Microbiota Colitis JujubeOral administration of Lactobacillus acidophilus 6074 fermented jujube juice can improve gut microbiota, alleviate intestinal inflammation, and reduce colon damage in mice.

Tremella aurantialba polysaccharides alleviate ulcerative colitis in mice by improving intestinal barrier via modulating gut microbiota and inhibiting ferroptosis
2024 Nov International Journal of Biological Macromolecules Peng G, Wang S, Zhang H, Xie F, Jiao L, Yuan Y, et al.
Experimental Study Animal Study Gut Microbiota Ulcerative Colitis Intestinal Barrier Snow FungusA polysaccharide from Tremella aurantialba improves ulcerative colitis symptoms by targeting epithelial cell ferroptosis and modulating the gut microbiota.

Effectiveness of a novel diet in attenuation of clinical activity of disease in patients with ulcerative colitis: a randomized, clinical trial
2024 Jun 14 Scientific Reports Narimani B, Sadeghi A, Daryani NE, Shahrokh S, Nilghaz M, Ghods M, et al.
Randomised Controlled Trial Low FODMAP Ulcerative ColitisA combined Mediterranean, low-FODMAP diet along with partial enteral nutrition has shown promise in reducing ulcerative colitis activity and improving patients' quality of life.
Carrageenan as a Potential Factor of Inflammatory Bowel Diseases
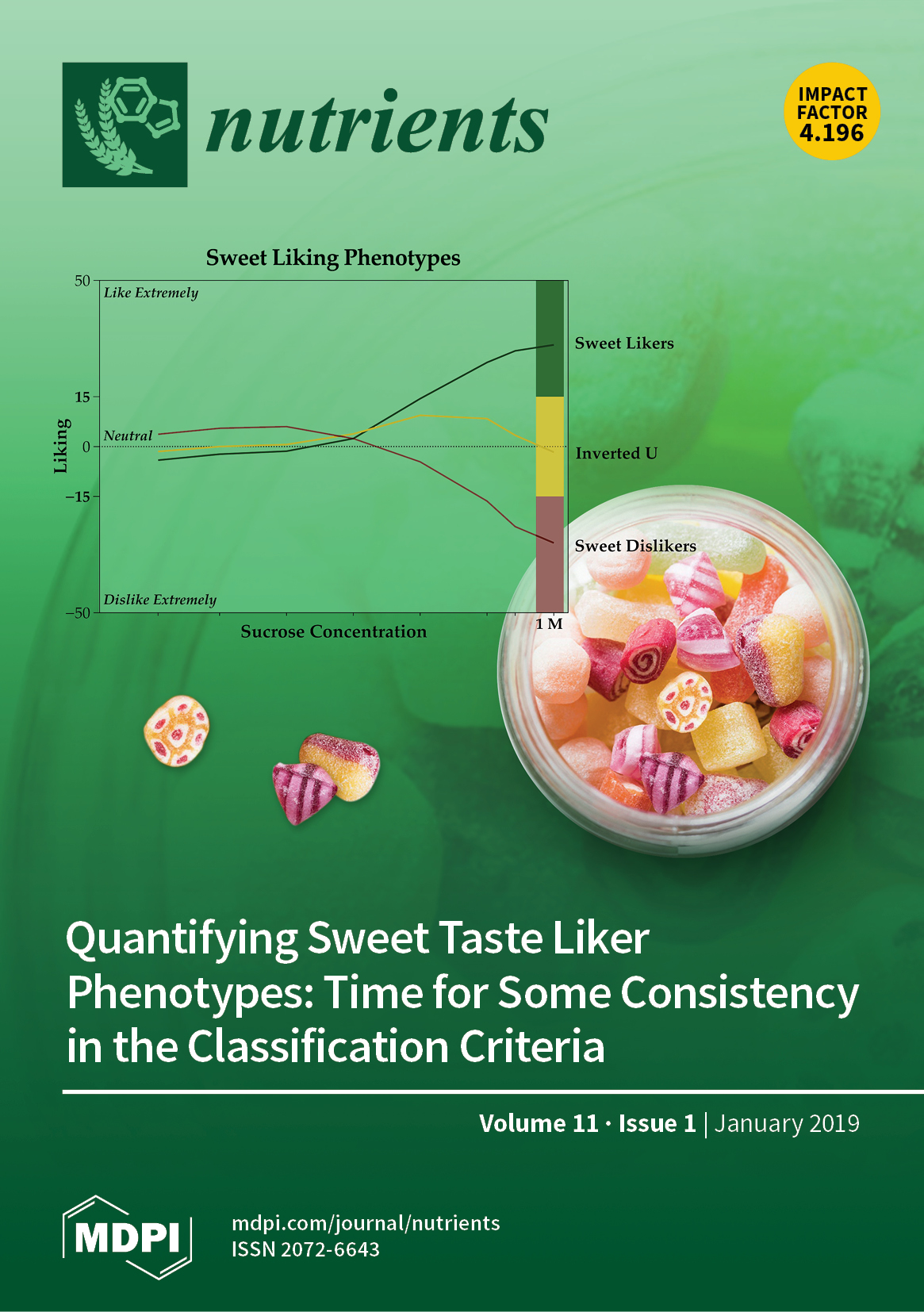
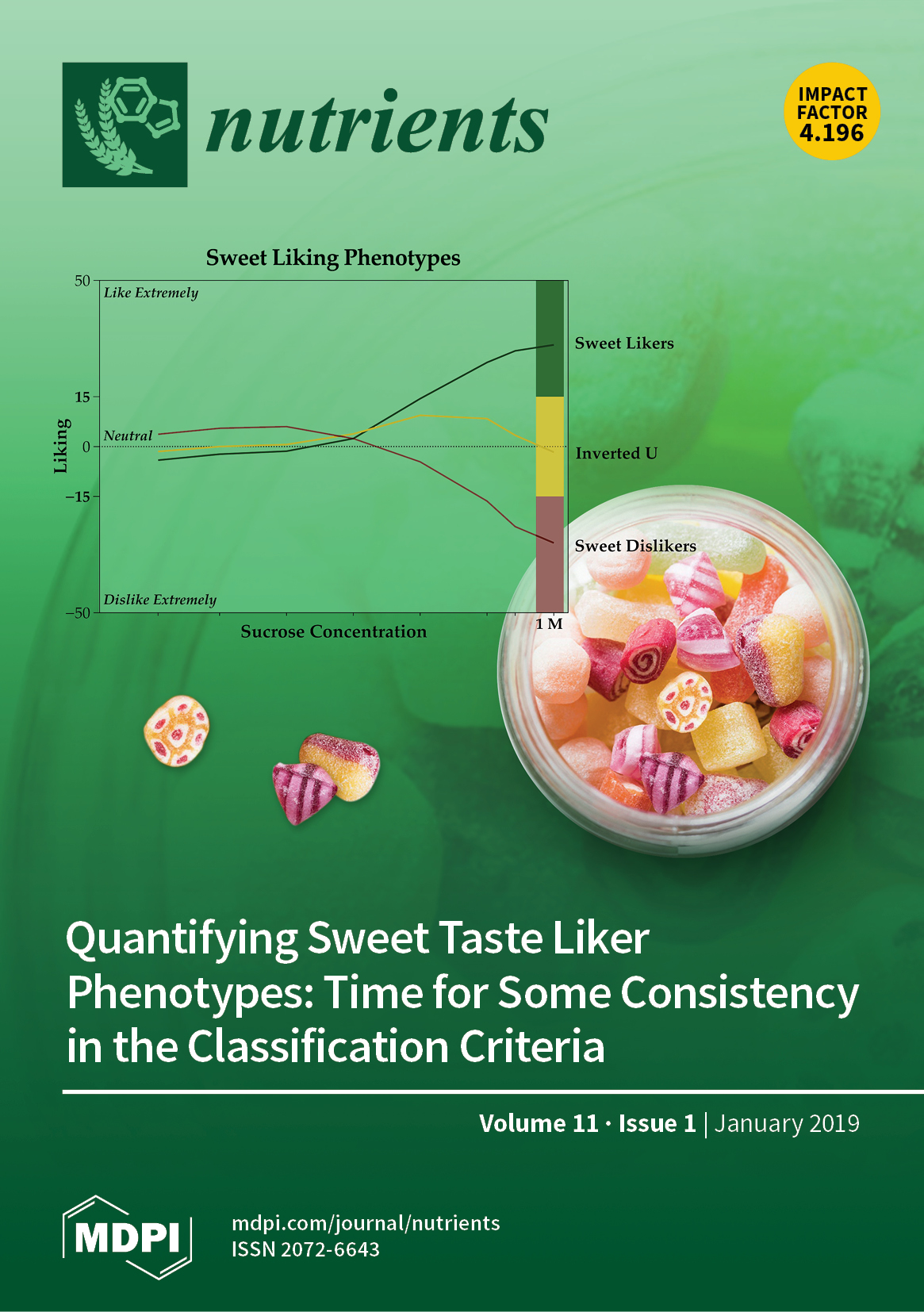
2024 Apr 30 Nutrients Komisarska P, Pinyosinwat A, Saleem M, Szczuko M
Animal Study Inflammatory Bowel Diseases CarrageenanCarrageenan, a common food additive, has dual aspects, being both useful in drug delivery and food printing, while potentially harmful via inducing intestinal inflammatory conditions.

Effects of acupuncture and moxibustion on ulcerative colitis: An overview of systematic reviews
2024 Mar Heliyon Wang D, Wang Q, Wang Y, Li T, Tian M
Systematic Review Moxibustion Acupuncture Ulcerative ColitisAcupuncture and moxibustion therapies have shown effectiveness in treating ulcerative colitis according to the summarised-findings of various systematic reviews and meta-analyses.
Research insights are moderated by the Research Hub team and offer an at-a-glance overview of interesting research findings.

2024 Molecular Nutrition & Food Research
Oral administration of Lactobacillus acidophilus 6074 fermented jujube juice can improve gut microbiota, alleviate intestinal inflammation, and reduce colon damage in mice.
Animal Study Gut Microbiota Jujube Lactobacillus
Lactobacillus acidophilus 6074 Fermented Jujube Juice Ameliorated DSS‐induced Colitis via Repairing Intestinal Barrier, Modulating Inflammatory Factors, and Gut Microbiota
Li H, Fan L, Yang S, Tan P, Lei W, Yang H, et al.

2024 International Journal of Biological Macromolecules
A polysaccharide from Tremella aurantialba improves ulcerative colitis symptoms by targeting epithelial cell ferroptosis and modulating the gut microbiota.
Experimental Study Gut Microbiota Intestinal Barrier Snow Fungus Ulcerative Colitis
Tremella aurantialba polysaccharides alleviate ulcerative colitis in mice by improving intestinal barrier via modulating gut microbiota and inhibiting ferroptosis
Peng G, Wang S, Zhang H, Xie F, Jiao L, Yuan Y, et al.

2024 Scientific Reports
A combined Mediterranean, low-FODMAP diet along with partial enteral nutrition has shown promise in reducing ulcerative colitis activity and improving patients' quality of life.
Randomised Controlled Trial Low FODMAP Ulcerative Colitis
Effectiveness of a novel diet in attenuation of clinical activity of disease in patients with ulcerative colitis: a randomized, clinical trial
Narimani B, Sadeghi A, Daryani NE, Shahrokh S, Nilghaz M, Ghods M, et al.
2024 Nutrients
Carrageenan, a common food additive, has dual aspects, being both useful in drug delivery and food printing, while potentially harmful via inducing intestinal inflammatory conditions.
Animal Study Carrageenan Inflammatory Bowel Diseases
Carrageenan as a Potential Factor of Inflammatory Bowel Diseases
Komisarska P, Pinyosinwat A, Saleem M, Szczuko M

2024 Heliyon
Acupuncture and moxibustion therapies have shown effectiveness in treating ulcerative colitis according to the summarised-findings of various systematic reviews and meta-analyses.
Systematic Review Acupuncture Moxibustion Ulcerative Colitis
Effects of acupuncture and moxibustion on ulcerative colitis: An overview of systematic reviews
Wang D, Wang Q, Wang Y, Li T, Tian M
Review Articles
Review articles summarise and critically evaluate the current state of research on a specific topic or field by synthesising multiple primary research studies.

Effects of acupuncture and moxibustion on ulcerative colitis: An overview of systematic reviews
2024 Mar Heliyon Wang D, Wang Q, Wang Y, Li T, Tian M
Systematic Review Moxibustion Acupuncture Ulcerative ColitisAcupuncture and moxibustion therapies have shown effectiveness in treating ulcerative colitis according to the summarised-findings of various systematic reviews and meta-analyses.
Efficacy and Safety of Different Acupuncture Therapies for Patients with Ulcerative Colitis:A Systematic Review And Network Meta-Analysis
2024 Jan SSRN Electronic Journal Zhang X, Yang S, Jin Y, Cheng X, Lu H, Wu H, et al.
Meta-Analysis Systematic Review Moxibustion Acupuncture Ulcerative ColitisDiverse acupuncture therapies, especially moxibustion, emerged as superior methods for alleviating ulcerative colitis symptoms in clinical practice.
Repairing the intestinal mucosal barrier of traditional Chinese medicine for ulcerative colitis: a review
2023 Oct 24 Frontiers in Pharmacology Zong Y, Meng J, Mao T, Han Q, Zhang P, Shi L
Theoretical Article Review Article Ulcerative ColitisTraditional Chinese medicine has been found to effectively treat ulcerative colitis by repairing various components of the damaged intestinal mucosal barrier.

Efficacy and safety of acupoint application in the treatment of ulcerative colitis: A systematic review and meta-analysis
2023 Aug 18 Medicine Tong Y, Yu Y, Yin S, Lin S, Chen Y, Su X
Meta-Analysis Systematic Review Ulcerative ColitisAcupoint application has been proven to be a safe and effective method for the treatment of ulcerative colitis.
Chinese herbal medicines for treating ulcerative colitis via regulating gut microbiota-intestinal immunity axis
2023 Apr Chinese Herbal Medicines Yang Y, Wang Y, Zhao L, Wang F, Li M, Wang Q, et al.
Review Article Gut Microbiota Ulcerative ColitisChinese herbal medicines could potentially relieve ulcerative colitis by moderating the gut microbiota and intestinal immunity loop.
Clinical Trials
Clinical trials are research studies that involve people and are conducted to evaluate the safety and efficacy of new treatments or interventions, such as drugs, medical devices, or behavioural therapies.

Effectiveness of a novel diet in attenuation of clinical activity of disease in patients with ulcerative colitis: a randomized, clinical trial
2024 Jun 14 Scientific Reports Narimani B, Sadeghi A, Daryani NE, Shahrokh S, Nilghaz M, Ghods M, et al.
Randomised Controlled Trial Low FODMAP Ulcerative ColitisA combined Mediterranean, low-FODMAP diet along with partial enteral nutrition has shown promise in reducing ulcerative colitis activity and improving patients' quality of life.
Anti-Inflammatory Diet Prevents Subclinical Colonic Inflammation and Alters Metabolomic Profile of Ulcerative Colitis Patients in Clinical Remission
2022 Aug 11 Nutrients Keshteli A, Valcheva R, Nickurak C, Park H, Mandal R, van Diepen K, et al.
Randomised Controlled Trial Anti-Inflammatory Ulcerative ColitisDietary modifications, combining increased intake of anti-inflammatory foods and decreased intake of pro-inflammatory foods, effectively impede subclinical inflammation in ulcerative colitis patients in clinical remission.
Randomised clinical trial: Efficacy and safety of Qing-Chang-Hua-Shi granules in a multicenter, randomized, and double-blind clinical trial of patients with moderately active ulcerative colitis
2021 Jul Biomedicine & Pharmacotherapy Shen H, Zhang S, Zhao W, Ren S, Ke X, Gu Q, et al.
Randomised Controlled Trial Qing Chang Hua Shi Ulcerative ColitisQing-Chang-Hua-Shi (QCHS) granules, a Chinese herbal formula, have shown significant efficacy in improving clinical remission and mucosal healing in moderately active ulcerative colitis patients.

The effects of extra virgin olive oil and canola oil on inflammatory markers and gastrointestinal symptoms in patients with ulcerative colitis
2020 Jan 03 European Journal of Clinical Nutrition Morvaridi M, Jafarirad S, Seyedian SS, Alavinejad P, Cheraghian B
Clinical Study Randomised Controlled Trial Ulcerative Colitis Extra Virgin Olive OilExtra virgin olive oil (EVOO) intake can reduce inflammatory markers and improve gastrointestinal symptoms in patients with Ulcerative Colitis.
A randomized trial of the effects of the no-carrageenan diet on ulcerative colitis disease activity
2017 Mar 31 Nutrition and Healthy Aging Bhattacharyya S, Shumard T, Xie H, Dodda A, Varady KA, Feferman L, et al.
Randomised Controlled Trial Carrageenan Ulcerative ColitisCarrageenan intake can lead to an earlier relapse in patients with ulcerative colitis who are in remission.
Study Protocols
Published study protocols are detailed plans that outline the objectives, methodology, statistical analyses, and organisation of a research study that have been made publicly available for others to review and use as a reference.
Presentation Slides

Animal Study
Oral administration of Lactobacillus acidophilus 6074 fermented jujube juice can improve gut microbiota, alleviate intestinal inflammation, and reduce colon damage in mice.
Li H, Fan L, Yang S, Tan P, Lei W, Yang H, Gao Z

Experimental Study
A polysaccharide from Tremella aurantialba improves ulcerative colitis symptoms by targeting epithelial cell ferroptosis and modulating the gut microbiota.
Peng G, Wang S, Zhang H, Xie F, Jiao L, Yuan Y, Ma C, Wu H, Meng Z

Randomised Controlled Trial
A combined Mediterranean, low-FODMAP diet along with partial enteral nutrition has shown promise in reducing ulcerative colitis activity and improving patients' quality of life.
Narimani B, Sadeghi A, Daryani NE, Shahrokh S, Nilghaz M, Ghods M, Shafiee M, Shahparvari MR, Hekmatdoost A
Animal Study
Carrageenan, a common food additive, has dual aspects, being both useful in drug delivery and food printing, while potentially harmful via inducing intestinal inflammatory conditions.
Komisarska P, Pinyosinwat A, Saleem M, Szczuko M

Systematic Review
Acupuncture and moxibustion therapies have shown effectiveness in treating ulcerative colitis according to the summarised-findings of various systematic reviews and meta-analyses.
Wang D, Wang Q, Wang Y, Li T, Tian M
Meta-Analysis
Diverse acupuncture therapies, especially moxibustion, emerged as superior methods for alleviating ulcerative colitis symptoms in clinical practice.
Zhang X, Yang S, Jin Y, Cheng X, Lu H, Wu H, Ji J
Theoretical Article
Traditional Chinese medicine has been found to effectively treat ulcerative colitis by repairing various components of the damaged intestinal mucosal barrier.
Zong Y, Meng J, Mao T, Han Q, Zhang P, Shi L

Meta-Analysis
Acupoint application has been proven to be a safe and effective method for the treatment of ulcerative colitis.
Tong Y, Yu Y, Yin S, Lin S, Chen Y, Su X
Review Article
Chinese herbal medicines could potentially relieve ulcerative colitis by moderating the gut microbiota and intestinal immunity loop.
Yang Y, Wang Y, Zhao L, Wang F, Li M, Wang Q, Luo H, Zhao Q, Zeng J, Zhao Y, Du F, Chen Y, Shen J, Wei S, Xiao Z, Wu X

Experimental Study
Goji berry leaves have stronger anti-colitis effects than mulberry leaves, ameliorating tissue damage and better regulating inflammatory responses and gut microbiota.
Yu C, Chen Y, Ahmadi S, Wu D, Wu J, Ding T, Liu D, Ye X, Chen S, Pan H
Meta-Analysis
Patients with ulcerative colitis (UC) experienced greater clinical improvement and fewer adverse effects when treated with a combination of Traditional Chinese and Western medicine compared to Western medicine alone.
Chen S, Ji G, Liu X, Yang M, Zhang Y, Cao J, Pan Y

Review Article
Polysaccharides from natural food sources like fungi and plants can significantly enhance intestinal health and prevent ulcerative colitis (UC) through various physiological activities.
Pan X, Yin M, Guo M, Niu X, Han L
Randomised Controlled Trial
Dietary modifications, combining increased intake of anti-inflammatory foods and decreased intake of pro-inflammatory foods, effectively impede subclinical inflammation in ulcerative colitis patients in clinical remission.
Keshteli A, Valcheva R, Nickurak C, Park H, Mandal R, van Diepen K, Kroeker K, van Zanten S, Halloran B, Wishart D, Madsen K, Dieleman L
Cohort Study
Higher consumption of ultra-processed food is linked to an increased risk of developing Crohn's disease, with no consistent connection observed with ulcerative colitis.
Lo CH, Khandpur N, Rossato SL, Lochhead P, Lopes EW, Burke KE, Richter JM, Song M, Ardisson Korat AV, Sun Q, Fung TT, Khalili H, Chan AT, Ananthakrishnan AN

Cohort Study
Shenling Baizhu San (SBS), combined with mesalamine, can treat ulcerative colitis effectively by changing gut microbiota structures and increasing tryptophan metabolite levels.
Jiao C, Zhang Q, Yang M, Ma J, Zhao X, Tang N, Dai M, Li Q, Jiang Z, Huang X, Zhang H, Sun L

Review Article
Chinese herbal medicine interventions, particularly those based on the Bai-Tou-Weng-Tang and Shen-Ling-Bai-Zhu-San formulas, show promise in treating Ulcerative Colitis.
Zhang X, Zhang L, Chan JCP, Wang X, Zhao C, Xu Y, Xiong W, Chung WC, Liang F, Wang X, Miao J, Bian Z
Review Article
Omega-3 fatty acids can help prevent and manage chronic inflammatory diseases, including ulcerative colitis and rheumatoid arthritis, through influencing gut microbiota.
Zorgetto-Pinheiro VA, Machate DJ, Figueiredo PS, Marcelino G, Hiane PA, Pott A, Guimarães RCA, Bogo D
Meta-Analysis
Probiotics combined with traditional Chinese medicine have shown higher rates of efficiency in the treatment of ulcerative colitis than when each is used individually.
Hu Y, Ye Z, She Y, Li L, Wu M, Qin K, Li Y, He H, Hu Z, Yang M, Lu F, Ye Q

Meta-Analysis
Traditional Chinese Medicine may potentially be a viable treatment option for ulcerative colitis, but its effectiveness varies depending on the method of administration applied.
Sun YX, Wang X, Liao X, Guo J, Hou WB, Wang X, Liu JP, Liu ZL
Randomised Controlled Trial
Qing-Chang-Hua-Shi (QCHS) granules, a Chinese herbal formula, have shown significant efficacy in improving clinical remission and mucosal healing in moderately active ulcerative colitis patients.
Shen H, Zhang S, Zhao W, Ren S, Ke X, Gu Q, Tang Z, Xie J, Chen S, Chen Y, Zou J, Zhang L, Shen Z, Zheng K, Liu Y, Gu P, Cheng J, Hu J, Zhu L

Systematic Review
Tremella fuciformis polysaccharides effectively reduce inflammation in ulcerative colitis, promoting healing by restoring intestinal and mucus barrier functions.
Xu Y, Xie L, Zhang Z, et al
Experimental Study
Two French natural mineral waters (NMW1 and NMW2) show anti-inflammatory effects and can reduce intestinal inflammation in mice with induced colitis.
Barnich N, Rodrigues M, Sauvanet P, Chevarin C, Denis S, Le Goff O, Faure-Imbert D, Hanh T, Roques CF, Chassaing B, Alric M
Network Pharmacology
Kushen-based traditional Chinese medicine formulations show considerable potential and effectiveness in treating ulcerative colitis with meaningful improvement in clinical remission rate.
Chen M, Ding Y, Tong Z

Meta-Analysis
Oral treatment with Six Gentlemen Decoction with Aucklandia and Amomum (SGDAA), a traditional Chinese medicine, significantly improves the treatment of Ulcerative colitis compared to conventional Western medicine.
Yuan H, Zhang T, Huang S, Zhou J, Park S

Clinical Study
Extra virgin olive oil (EVOO) intake can reduce inflammatory markers and improve gastrointestinal symptoms in patients with Ulcerative Colitis.
Morvaridi M, Jafarirad S, Seyedian SS, Alavinejad P, Cheraghian B
Review Article
The diet might influence the onset and pathophysiology of ulcerative colitis, and can potentially be used in its management.
Keshteli AH, Madsen KL, Dieleman LA

Experimental Study
Dietary supplementation with Goji berries enhances Bifidobacteria and butyrate-producing bacteria growth, resulting in potential preventative effects against colitis.
Kang Y, Yang G, Zhang S, Ross CF, Zhu MJ

Randomised Controlled Trial
Carrageenan intake can lead to an earlier relapse in patients with ulcerative colitis who are in remission.
Bhattacharyya S, Shumard T, Xie H, Dodda A, Varady KA, Feferman L, Halline AG, Goldstein JL, Hanauer SB, Tobacman JK
Executive Summary
Write an executive summary in the form of a blog article on the topic of "Research into Chinese medicine treatment for Colitis" summarising the research below and using language that can be easily understood by patients and avoiding medical jargon using a professional and caring tone of voice.
Write an executive summary in the form of a blog article on the topic of "Researched Chinese medicine treatments for Colitis" summarising the research below in an objective and easy to understand way, and using language that can be easily understood by patients. Group the article into Chinese medicine treatments first, followed by nutrition and other treatments. Avoid using medical jargon and use a professional and caring tone of voice.
Write me a concise but easy to understand executive summary on the topic of "Chinese medicine treatments for Colitis" based on the following research that I will give you. Your summary should be 2 paragraphs long in Australian English spelling and include references to the studies.
A Animal Study published in 2024 in the journal Molecular Nutrition & Food Research found that Oral administration of Lactobacillus acidophilus 6074 fermented jujube juice can improve gut microbiota, alleviate intestinal inflammation, and reduce colon damage in mice. The study used jujube juice as the substrate fermented by L. acidophilus 6074 to observe its effects on gut microbiota, intestinal barrier function, oxidative stress, and inflammatory factors in mice with colitis. The process of fermentation caused significant changes in the compounds of the juice, particularly in organic acids and free amino acids. A high dose of the juice demonstrated significant improvements in overall colitis markers, including the physical condition of the colon and disease activity. Upon administering the fermented jujube juice, it was observed that the treatment promoted the reinforcement of the colonic mucosal barrier, boosting the expression of various tight junction proteins. Moreover, it inhibited the production of proinflammatory factors and reduced oxidative stress, thereby mitigating colon damage. The gut microbiota composition shifted as a result, demonstrating an increase in beneficial bacteria, a boost in short-chain fatty acids, and a reduction in harmful microorganisms. These findings indicate that the fermented juice can restore the balance in gut microbiota altered by intestinal inflammation and lessen the impact of colitis.
A Experimental Study published in 2024 in the journal International Journal of Biological Macromolecules found that A polysaccharide from Tremella aurantialba improves ulcerative colitis symptoms by targeting epithelial cell ferroptosis and modulating the gut microbiota. The methodology used in this research involved isolating TA 2-1, a specific polysaccharide from Tremella Aurantialba, and studying its effects on ulcerative colitis. This was done by introducing it to Caco-2 cells that were undergoing ferroptosis and assessing its impact on cell viability. The influence of TA 2-1 was also examined in mice with artificially induced ulcerative colitis, verifying its ameliorating effects in an in-vivo context. The structure of TA 2-1 and its components were analysed and the polysaccharide's interaction with gut microbiota was explored to understand how it might modulate symptoms or prevent cell death. The results of this study showed that TA 2-1 does not only decrease the rate of cell death in epithelial cells undergoing ferroptosis, but it also repairs the intestinal barrier by upregulating specific proteins such as claudin-1 and zonula occludens-1. TA 2-1 was also found to suppress lipid peroxidation, thus inhibiting ferroptosis. Further investigation revealed that TA 2-1 may alleviate ulcerative colitis by influencing the composition or metabolites of gut microbiota. This research offers promising insight into the potential of TA 2-1 in treating ulcerative colitis.
A Randomised Controlled Trial published in 2024 in the journal Scientific Reports found that A combined Mediterranean, low-FODMAP diet along with partial enteral nutrition has shown promise in reducing ulcerative colitis activity and improving patients' quality of life. In the study, fifty patients with active, mild to moderate ulcerative colitis were randomly allotted one of two diets: a combined Mediterranean, low-FODMAP diet supplemented with partial enteral nutrition, or a standard diet. These diets were implemented for a duration of 6 weeks. Before and after the intervention, various indicators of the patients' conditions were measured. These variables included a disease activity index, the patients' quality of life, and concentrations of various inflammatory and oxidative stress factors in the blood. All of these were measured using tested and trustworthy questionnaires, in conjunction with blood sampling. The combined diet was found to result in significantly decreased disease activity index values, compared to both the control diet and the baseline data. Simultaneously, patients on the combined diet reported greater enhancements in their quality of life, compared to both the control group and the initial data. Lastly, the serum level of a protein called "high sensitive C-reactive protein," known to be a general marker of inflammation within the body, was found to be reduced in the combined diet group. However, changes in the serum total antioxidant capacity were found to be statistically insignificant across both groups.
A Animal Study published in 2024 in the journal Nutrients found that Carrageenan, a common food additive, has dual aspects, being both useful in drug delivery and food printing, while potentially harmful via inducing intestinal inflammatory conditions. This study investigates the dual roles of carrageenan, a naturally occurring polysaccharide. It is used in creating edible films and encapsulating drugs, and has potential uses in food printing. Moreover, it can regulate the composition of intestinal microflora, including promoting the increase of Bifidobacterium bacteria. The research shines a light on the harmful side of carrageenan as well by focusing on its interactive effects with intestinal microflora, mucous barrier, and proinflammatory pathways. The study reveals that carrageenan negatively alters intestinal microflora, triggering a breakdown of the mucus barrier, leading to an inflammatory response. This response occurs due to activation of the pro-inflammatory nuclear factor kappa-light-chain-enhancer pathway in the epithelial cells, likely via the mechanism of TLR4 receptor activation, alteration in macrophage activity, production of proinflammatory cytokines, and activation of innate immune pathways. Carrageenan's influence also led to increased levels of Bacteroidetes bacteria, alongside reducing short-chain fatty acid-producing bacteria, ultimately damaging the integrity of the intestinal membrane and reducing the mucin layer. The study finds that those with intestinal inflammation disorders, like Crohn's disease and ulcerative colitis, are particularly vulnerable to these harmful effects.
A Systematic Review published in 2024 in the journal Heliyon found that Acupuncture and moxibustion therapies have shown effectiveness in treating ulcerative colitis according to the summarised-findings of various systematic reviews and meta-analyses. Methodology: This evaluative study used an extensive and systematic methods to search data from seven different databases. The selected data were further refined by using different screening and evaluation frameworks like AMSTAR-2, PRISMA, ROBIS, and GRADE systems. These were used to determine the methodological quality, reporting quality, risk of bias, and the quality of evidence in the selected studies. Discussion of results: After critical evaluation, the study found ten relevant reviews and analyses that showed potential for acupuncture and moxibustion therapies being effective in ulcerative colitis treatment. However, many the identified studies were reported to have several problems in their overall design and quality of outcomes. The researchers therefore stress caution when interpreting these results due to the lack of high-quality evidence in the existing studies.
A Meta-Analysis published in 2024 in the journal SSRN Electronic Journal found that Diverse acupuncture therapies, especially moxibustion, emerged as superior methods for alleviating ulcerative colitis symptoms in clinical practice. Methodology: The researchers carried out a systematic review and network meta-analysis of clinical efficacy of various acupuncture therapies for ulcerative colitis patients. They accomplished this by sourcing for Clinical Randomized Controlled trial articles from databases such as PubMed, Embase, Cochrane Library, and other data knowledge service platforms, all of which were independently reviewed by two researchers. Several quality assessments were made through Review Manager software, and the meta-analysis was conducted with Stata 16 software. Interventions examined in the analysis included acupuncture, moxibustion, acupoint catgut embedding, and combinations of these therapies with Western medicine. Discussion of results: 52 articles encompassing 3924 patients participated in randomized control trials. The investigation revealed a range of interventions, including different acupuncture therapies and combinations of these therapies with Western medicine. Namely, moxibustion, either on its own or combined with Western medicine, consistently surfaced as top-ranked for overall effectiveness and specific outcomes. Moreover, moxibustion displayed impressive performance in reducing adverse reactions and recurrence rates. Thus, various acupuncture therapies were confirmed as safe and effective for the treatment of ulcerative colitis, with moxibustion emerging as the most effective.
A Theoretical Article published in 2023 in the journal Frontiers in Pharmacology found that Traditional Chinese medicine has been found to effectively treat ulcerative colitis by repairing various components of the damaged intestinal mucosal barrier. In the methodology, the study sought to uncover the efficacy of Traditional Chinese medicine (TCM) in treating ulcerative colitis (UC). The research began by acknowledging the key role that damage to the intestinal mucosal barrier plays in the development of UC. It then explored how TCM could combat UC by protecting and repairing various aspects of this barrier including the physical, chemical, immune, and biological barrier. In the results discussion, it was discovered that TCM not only increases the number of intestinal epithelial cells, tight junction proteins, and mucins, but also encourages the proliferation of intestinal stem cells, restores the abundance of the intestinal microbiota, and modulates immunity in the gut. Moreover, the study identified several upstream proteins and signaling pathways that were activated in the process. This gives hope to future treatment plans for UC using TCM, with the study providing a fundamental theoretical basis and new ideas for future investigations.
A Meta-Analysis published in 2023 in the journal Medicine found that Acupoint application has been proven to be a safe and effective method for the treatment of ulcerative colitis. The methodology incorporated a systematic review of various databases including China National Knowledge Infrastructure, Chinese Biology Medicine, VIP, Wanfang, Embase, PubMed, the Cochrane Library and Web of Science up to July 2022 to find published randomized controlled trials on the use of acupoint application in treating ulcerative colitis. Meta-analysis and trial sequential analysis were then performed on the selected studies. The results from the 13 analyzed trials involving a total of 878 cases revealed that the use of acupoint application improved the rates of effective clinical comprehensive and syndrome in ulcerative colitis treatment compared to conventional western medicine. The method also showed advantages in increasing interleukin-4 and reducing interferon-gamma. Also noted was that there were no variances seen regarding colonoscopy, pathological examination, and reaction rates when compared with traditional methods. The quality of the evidence used for these conclusions varied, with some being of moderate quality and others deemed low or very low quality.
A Review Article published in 2023 in the journal Chinese Herbal Medicines found that Chinese herbal medicines could potentially relieve ulcerative colitis by moderating the gut microbiota and intestinal immunity loop. The study emphasizes on the possible use of Chinese herbal medicines, which include single herbs, herbal formulas and derived constituents, in treating ulcerative colitis (UC), a recurring inflammatory bowel disease. With a focus on how these medicines interact with and modify the gut microbiota, the mechanism involves regulating the intestinal homeostasis to counter UC. It deals with balancing microbial dysbiosis, or the imbalance of microbes in the body, and abnormal gut immunity, two key initiators of inflammatory responses in UC. The paper reviews several clinical trials which have been conducted, all exhibiting the effectiveness of Chinese herbal medicines on patients diagnosed with UC. In the trials, these derived substances have shown a protective effect against UC, offering the potential possibility of them being explored as conventional methods of UC treatments in the future. Not every trial has resulted in absolute success, but the overall results are promising and indicate a robust potential direction for UC treatment science.
A Experimental Study published in 2023 in the journal Food & Function found that Goji berry leaves have stronger anti-colitis effects than mulberry leaves, ameliorating tissue damage and better regulating inflammatory responses and gut microbiota. The research entailed a comparative study conducted on goji berry and mulberry leaves versus their respective fruits. To determine their anti-colitis effects, the experiment was administered to C57BL/6N mice that had been induced with colitis through dextran-sulfate-sodium. Through the utilization of measures such as ELISA and western blotting analysis, researchers were able to observe how each leaf versus its corresponding fruit ameliorated colitic symptoms, tissue damage, and was able to influence the overproduction of certain pro-inflammatory cytokines. The results showed that both the goji berry leaf and fruit significantly reduced symptoms of colitis and improved tissue damage while the mulberry leaf did not show similar improvements. The goji berry leaf exhibited the strongest performance in restraining the overproduction of pro-inflammatory cytokines and further repairing the damaged colonic barrier. It also effectively adjusted gut microbiota equilibrium by increasing beneficial bacteria and decreasing harmful ones. The berries and leaves similarly restored certain dietary fibers to alleviate inflammation, but the mulberry leaf did not achieve this for butyrate. This is the first report to provide a comprehensive contrast of anti-colitis effects between the leaves and fruits of goji and mulberry.
A Meta-Analysis published in 2022 in the journal Pharmacological Research - Modern Chinese Medicine found that Patients with ulcerative colitis (UC) experienced greater clinical improvement and fewer adverse effects when treated with a combination of Traditional Chinese and Western medicine compared to Western medicine alone. With an aim to assess the effectiveness and safety of combined Traditional Chinese and Western medicine (referred as ITCMWM hereafter) in treating ulcerative colitis, a systematic review was conducted following a registered protocol. Data was sourced from numerous databases including PubMed, Cochrane Library, Embase, the Chinese Biomedical Literature Database (CBM), the China National Knowledge Infrastructure (CNKI), and Wanfang Data. The review incorporated only randomized controlled trials comparing ITCMWM with stand-alone Western medicine. A total of 3957 patients from 38 studies, equally divided into the ITCMWM group and control group, were considered, and the risk ratios were calculated. The results from the aggregated studies show that patients in the ITCMWM group reported a significantly better clinical outcome and witnessed fewer adverse events when compared to patients on stand-alone Western medicine. It was observed that the combination of both Traditional Chinese and Western treatments clearly outperformed Western medicine treatment alone in terms of overall effectiveness on ulcerative colitis. Additionally, the safety level was nearly equal for both treatment methods.
A Review Article published in 2022 in the journal Journal of Functional Foods found that Polysaccharides from natural food sources like fungi and plants can significantly enhance intestinal health and prevent ulcerative colitis (UC) through various physiological activities. The study primarily focused on the role of natural food polysaccharides in promoting intestinal health. Derived from sources like edible fungi and plants, these substances exhibit remarkable potential in preventing UC, a common inflammatory bowel disease. The researchers have investigated their action mechanism which mainly involved promoting beneficial bacteria, reducing harmful bacteria, increasing Short Chain Fatty Acids (SCFA) content, and exerting prebiotic effects. The polysaccharides' ability to prevent UC by blocking certain cellular pathways, regulating tight junctions, repairing the intestinal barrier function, inhibiting oxidative stress, and mitigating oxidative damage to the colon tissue was also explored. The structure of these polysacaccharides and their relationship to the prevention of UC were however not covered fully in the study. The obtained results deliver a profound understanding of the preventive effects of natural food polysaccharides on UC. Their capacity to promote beneficial bacteria while reducing the harmful species has been emphasized. They were also found to increase the content of SCFAs and act as prebiotics. Additionally, their role in blocking certain signaling pathways and thus preventing oxidative stress and damage further presents them as effective defense agents against UC. The observations related to the relationship between the structure of these polysaccharides and the prevention of UC were less conclusive. This study, however, did note a lacking of clear connection between the molecular weight of polysaccharides and their preventive effects, leaving room for future extensive study in this area.
A Randomised Controlled Trial published in 2022 in the journal Nutrients found that Dietary modifications, combining increased intake of anti-inflammatory foods and decreased intake of pro-inflammatory foods, effectively impede subclinical inflammation in ulcerative colitis patients in clinical remission. The study conducted a 6-month open-label, randomized, placebo-controlled trial on adult patients with ulcerative colitis who were in clinical remission. The patients were randomly assigned to follow either an Anti-inflammatory Diet (AID) or Canada’s Food Guide (CFG). The AID was designed to raise the consumption of dietary fiber, probiotics, antioxidants, and omega-3 fatty acids, while reducing the intake of red meat, processed meat, and added sugars. Stool, urine, and serum samples were collected for fecal calprotectin and microbial analysis as well as metabolomic analysis at both the study's start and endpoint. A total of 53 patients were randomized in the study. The evaluation of the patients’ response to the intervention showed a higher subclinical response in the AID group. Patients in the AID group were found to have a higher intake of specific nutrients and foods such as zinc, phosphorus, selenium, yogurt, and seafood compared to the control group. The AID adherence was related to significant changes in the metabolome, with a decrease in fecal acetone and xanthine levels and an increase in fecal taurine and urinary carnosine and p-hydroxybenzoic acid levels. The AID subjects also exhibited increases in specific fecal bacterial families. In conclusion, dietary modifications involving the increased intake of anti-inflammatory foods combined with a decreased intake of pro-inflammatory foods were associated with metabolic and microbial changes and were effective in preventing subclinical inflammation in these patients.
A Cohort Study published in 2022 in the journal Clinical Gastroenterology and Hepatology found that Higher consumption of ultra-processed food is linked to an increased risk of developing Crohn's disease, with no consistent connection observed with ulcerative colitis. A prospective cohort study was conducted using three nationwide cohorts of health professionals in the United States. The study utilized self-reported consumption of ultra-processed foods to assess its association with the risk of Crohn's disease and ulcerative colitis. It involved 245,112 participants and spanned several years of observation. The analysis primarily leveraged Cox proportional hazards models to estimate hazard ratios for Crohn's disease and ulcerative colitis while adjusting for potential confounding factors. The study observed a total of 369 cases of Crohn's disease and 488 cases of ulcerative colitis over the period of follow-up. The participants in the highest quartile of ultra-processed food consumption experienced a noteworthy surge in the risk of developing Crohn's disease. Ultra-processed breads, breakfast foods, frozen or shelf-stable ready-to-eat or heat meals, and certain spreads and gravies showed the strongest positive correlations with Crohn's disease risk. However, no clear association was seen between ultra-processed food intake and the incidence of ulcerative colitis.
A Cohort Study published in 2022 in the journal Journal of Ethnopharmacology found that Shenling Baizhu San (SBS), combined with mesalamine, can treat ulcerative colitis effectively by changing gut microbiota structures and increasing tryptophan metabolite levels. The methodology involved conducting a prospective cohort study to explore the potential therapeutic effects of SBS, used as a complementary medicine with mesalamine, on ulcerative colitis patients. There were 48 patients included in the study, out of which 24 were a part of the control group and given just mesalamine, while the remaining patients in the experimental group were administered mesalamine along with SBS. The efficacy of these treatments was evaluated after an elapsed period of 8 weeks. The study utilized procedures like 16S rRNA sequencing to observe the structures of gut microbiota (GMB), and UPLC-MS/MS to analyze microbial tryptophan metabolites. In terms of results discussion, the study noticed that the combination of SBS and mesalamine significantly enhanced the clinical symptoms of ulcerative colitis. This was observed through mucosal healing and reduced damage to the colon that the medicinal combination induced. The research also highlighted a novel discovery, the alteration of gut microbiota structures, and an observable increase in microbial levels of tryptophan metabolites when both SBS and mesalamine were used. This led to the conclusion that SBS acted as an effective supplementary therapy to the standard treatment, easing ulcerative colitis through an identified GMB-tryptophan metabolite axis.
A Review Article published in 2022 in the journal Chinese Medicine found that Chinese herbal medicine interventions, particularly those based on the Bai-Tou-Weng-Tang and Shen-Ling-Bai-Zhu-San formulas, show promise in treating Ulcerative Colitis. This study analyzed Ulcerative Colitis clinical trials that used Chinese Herbal Medicine (CHM) interventions by systematically searching seven electronic databases for articles published in English and Chinese until November 25, 2020. The focus was on different CHM treatments, including both single herbs and CHM formulas. Descriptive statistics were utilized to portray the characteristics of these studies, along with collecting commonly Chinese Medicine (CM) patterns of UC and frequently used CHM herbs and formulas. The data from a total of 2311 studies were compiled, most of which were Randomized Controlled Trials (RCTs) that utilized CHM formulas. Findings revealed that the most commonly reported CM pattern in UC was 'Large Intestine Dampness-Heat', with 'Spleen Deficiency' being the basic CM pattern-type reported. Top CHM treatment formulas included Bai-Tou-Weng-Tang and Shen-Ling-Bai-Zhu-San. The most frequently used single medicinals were Huang Lian and Bai Zhu. Common Western medicine compounds used in tandem with CHM treatments were Sulfasalazine and Mesalazine.
A Review Article published in 2022 in the journal Journal of Medicinal Food found that Omega-3 fatty acids can help prevent and manage chronic inflammatory diseases, including ulcerative colitis and rheumatoid arthritis, through influencing gut microbiota. The study primarily encompasses a review of both experimental and clinical studies on the influence of omega-3 fatty acids on chronic inflammatory conditions, with the attention being specifically focused on those diseases with an autoimmune background. The study highlights the role of these fatty acids in maintaining bodily homeostasis, as well as the enzymatic processes they trigger within the body upon ingestion. Natural sources of omega-3 are also explored, emphasizing the importance of maintaining a healthy and balanced diet. In their exploration of omega-3's impact on inflammatory conditions, the researchers revisit the pathogenesis of ulcerative colitis and rheumatoid arthritis under the theoretical approach of gut microbiota dysbiosis. This approach emphasizes the role of the gut in maintaining health and identifies how imbalances can contribute to the development and persistence of these conditions. The researchers propose that omega-3 fatty acids are able to prevent and control these conditions, which are significant contributors to global chronic health burden and can lead to severe complications and disabilities if not treated. The potential of omega-3's to prevent severe illness in cases of COVID-19 infection through immune system modulation and control of the inflammatory process is also briefly explored.
A Meta-Analysis published in 2022 in the journal Frontiers in Pharmacology found that Probiotics combined with traditional Chinese medicine have shown higher rates of efficiency in the treatment of ulcerative colitis than when each is used individually. For the methodology, the researchers utilized a comprehensive search of multiple databases such as Pubmed, EMBASE, Cochrane library, China Academic Journals, Wan-fang database, Chinese biomedical literature service system, and Chinese Science and Technology Journals. They designed subgroup analysis in alignment with distinct control drugs, treatment lengths, and types of probiotics, using Review Manager software for statistical analysis. In discussing the results, the study analyzed fourteen original studies containing over a thousand patients. It concluded that the combination of probiotics with traditional Chinese medicine was more effective than 5-aminosalicylic acid, probiotics, or traditional Chinese medicine used individually. Further, this combination was found to suppress intestinal inflammation, diminish the frequency of recurrence, and lower the occurrence of adverse events. The results indicated that a mixture of different probiotics was more effective than a single strain.
A Meta-Analysis published in 2021 in the journal BMC Complementary Medicine and Therapies found that Traditional Chinese Medicine may potentially be a viable treatment option for ulcerative colitis, but its effectiveness varies depending on the method of administration applied. The authors conducted an extensive electronic literature search across six databases to find systematic reviews about the use of various Chinese medicine therapies for ulcerative colitis. They evaluated the reviews based on the methodology used for assessing their quality. Nine interventions fit the eligibility criteria from the 73 systematic reviews used for the study. It was found that the disease stages of patients with ulcerative colitis ranged greatly and therefore, influenced the outcomes of various treatment approaches. The authors found that the results mostly favored the method of intervention used, with oral administration combined with an enema being the most widely preferred administration route. Notably, many of the reviews didn't report essential factors such as the disease's location, the classification, and the intervention's route of administration. The current evidence indicates that while TCM could be a treatment for UC, it should be applied cautiously due to these inconsistencies.
A Randomised Controlled Trial published in 2021 in the journal Biomedicine & Pharmacotherapy found that Qing-Chang-Hua-Shi (QCHS) granules, a Chinese herbal formula, have shown significant efficacy in improving clinical remission and mucosal healing in moderately active ulcerative colitis patients. The double-blind, randomized and placebo-controlled study was performed across multiple centers, involving patients with moderately active ulcerative colitis who had been unresponsive to mesalazine therapy for a month. The participants were randomly divided into groups, where one group received a daily dose of 125g QCHS granules along with continual 5-Aminosalicylate(5-ASA) therapy, and the other group received a placebo with the same color, taste and texture as QCHS granules, also with 5-ASA therapy. The interpretation of the reported results revealed that both clinical remission and response were observed more substantially in the group treated with QCHS granules compared to the placebo group. Moreover, a higher rate of remission in mucus/bloody stools was seen in patients treated with QCHS granules versus the placebo. Overall, the adverse event rates did not significantly deviate between the QCHS granule and the placebo groups, indicating a similar level of safety for both treatments.
A Systematic Review published in 2021 in the journal International Journal of Biological Macromolecules found that Tremella fuciformis polysaccharides effectively reduce inflammation in ulcerative colitis, promoting healing by restoring intestinal and mucus barrier functions. In this study, two models were utilized to investigate the impacts of Tremella fuciformis polysaccharides on ulcerative colitis: a dextran sodium sulfate-induced mice model and a lipopolysaccharide-stimulated model using Caco-2 cells. First, the dextran sodium sulfate-induced mice ulcerative colitis model was administered with the Tremella fuciformis polysaccharides. Effects were observed across several indicators such as body weight, colon length, and thickness, as well as intestinal permeability. Following that, histopathological analysis and electron microscope examinations helped delve deeper into the relationship, uncovering a reduction in inflammatory cell infiltration and a restoration of the intestinal epithelial barrier integrity. The lipopolysaccharide-stimulated Caco-2 cells model was used to further understand the role of these polysaccharides in reducing expressions of pro-inflammatory cytokines and increasing expressions related to intestinal barrier and mucus barrier.
A Experimental Study published in 2021 in the journal International Journal of Molecular Sciences found that Two French natural mineral waters (NMW1 and NMW2) show anti-inflammatory effects and can reduce intestinal inflammation in mice with induced colitis. The study investigated the anti-inflammatory effects of two French natural mineral waters (NMWs) - NMW1 (rich in calcium, magnesium, sodium, carbon, and iron) and NMW2 (mainly bicarbonate) - on intestinal inflammation. Intestinal epithelial cells were stimulated with heat-inactivated Escherichia coli or hydrogen peroxide and then treated with NMWs. Additionally, moderate colitis was induced in Balbc/J mice using 1% dextran sulfate sodium. These mice were then given either NMW1, NMW2, or control water. The study assessed general symptoms, histological features of colitis, fecal lipocalin-2 levels, pro-inflammatory KC cytokine levels, and the global mucosa-associated microbiota. Both NMW1 and NMW2 showed anti-inflammatory effects in treated intestinal cells. In the colitis-induced mice, NMW1 notably reduced inflammation, evidenced by lower disease activity scores, reduced fecal lipocalin-2, decreased release of pro-inflammatory KC cytokines, and smaller intestinal epithelial lesions. NMW1 also helped in maintaining the normal state of mucosa-associated microbiota. These findings suggest the potential of these NMWs in managing inflammatory bowel disease through modulating gut microbiota.
A Network Pharmacology published in 2020 in the journal Frontiers in Pharmacology found that Kushen-based traditional Chinese medicine formulations show considerable potential and effectiveness in treating ulcerative colitis with meaningful improvement in clinical remission rate. In the study, researchers sourced multiple databases, specifically PubMed, EMBASE, Chinese Biomedical Literature database, China National Knowledge Infrastructure database, Chongqing VIP Information database, and Wanfang database, to find articles published from January 2000 to July 2020. These articles focused on randomized controlled trials using Kushen-based traditional Chinese medicine formulations for ulcerative colitis treatment. Additionally, they utilized a network pharmacology approach to discern the potential pathways of Kushen's influence against ulcerative colitis. Regarding the results, eight randomized controlled trials encompassing a total of 983 subjects were analyzed. When compared to subjects treated with standard therapy, patients who underwent treatment with Kushen-based formulations showed an increased clinical remission rate alongside a decreased incidence of adverse events. A detailed component-target-pathway network associated with Kushen treatment against ulcerative colitis was established. This highlighted five primary components, three primary targets, and one crucial therapeutic pathway.
A Meta-Analysis published in 2020 in the journal European Journal of Integrative Medicine found that Oral treatment with Six Gentlemen Decoction with Aucklandia and Amomum (SGDAA), a traditional Chinese medicine, significantly improves the treatment of Ulcerative colitis compared to conventional Western medicine. In the method of this research, Randomized controlled trials (RCTs) spanning the period from January 1960 to October 2019 were analyzed. These trials examined the use of the traditional Chinese medicine in question for treating ulcerative colitis. This extensive data was drawn from numerous scientific and medical databases in English, Korean, and Chinese. The resulting information was then processed through a software named RevMan 5.3 to conduct a meta-analysis. Furthermore, the studies were scrutinized based on their homogeneity and the odds ratios and confidence intervals were evaluated for accuracy and validity of each. In the exploration of the results, seven metanalysed studies (involving a total of 614 colitis patients) showed that the traditional Chinese medicine SGDAA had a significantly greater effect in treating ulcerative colitis than conventional western medicine. This conclusion was drawn from the comparative analysis of the SGDAA group (consisting of 308 patients) and the control group (composed of 306 patients receiving conventional Western medicine or another Chinese medicine). The analysis showed the SGDAA treatment was significantly more effective especially when the treatment exceeded 4 and 12 weeks. The beneficial impact of the SGDAA treatment in ulcerative colitis was seen in the forms of effective response and curative response.
A Clinical Study published in 2020 in the journal European Journal of Clinical Nutrition found that Extra virgin olive oil (EVOO) intake can reduce inflammatory markers and improve gastrointestinal symptoms in patients with Ulcerative Colitis. In the methodology of this study, forty patients suffering from Ulcerative Colitis participated in a crossover clinical trial, where the effects of extra virgin olive oil were compared with canola oil as part of their diet. Blood samples were collected before and after a 20-day intervention period, and measures such as disease activity and gastrointestinal symptoms were evaluated using established rating scales. In terms of results, the consumption of EVOO showed a significant decrease in recognized inflammatory markers. Furthermore, symptoms such as bloating, constipation, urgent bowel movements, and incomplete bowel evacuation were reported to have been significantly reduced following the consumption of EVOO. Therefore, this study suggests that extra virgin olive oil can offer significant benefits as a complementary medicine in the treatment of Ulcerative Colitis.
A Review Article published in 2019 in the journal Nutrients found that The diet might influence the onset and pathophysiology of ulcerative colitis, and can potentially be used in its management. The methodology used in reviewed studies relies typically on both epidemiological and experimental approaches to examine the relationship between diet and the onset and progression of ulcerative colitis. A combination of observational data from patients and well-structured randomized control trials have been undertaken, investigating both the potential causative effects of diet and its role in symptom management. In discussing the results, it is suggested that dietary factors do play a significant role in both the onset and the progression of ulcerative colitis. Though more data is needed through further trials, preliminarily, the manipulation of diet appears to have potential in managing the disease, indicating that dietary changes could either alleviate symptoms or trigger disease relapse. This points to an important role of diet in the approach to ulcerative colitis, a significant divergence from previous understandings of the disease.
A Experimental Study published in 2018 in the journal Molecular Nutrition & Food Research found that Dietary supplementation with Goji berries enhances Bifidobacteria and butyrate-producing bacteria growth, resulting in potential preventative effects against colitis. In this study, two groups of IL-10-deficient mice were used, with one group kept on a standard rodent diet and the other supplemented with a Goji berry diet, accounting for 1% of the dry feed's weight. These diets were maintained for 10 weeks. Colonic tissues and fecal contents were collected and analysed after this period. In the Goji supplemented group, there was a noticeable decrease in colonic pathobiological scores, a reduced mRNA expression of Il17a and Tgfb1, and an increase in Muc1 expression and fecal IgA content. Goji supplementation was found to increase the Actinobacteria phylum, leading to a surge in Bifidobacteria in the gut microbiota. Dietary Goji also promoted the growth of butyrate-producing bacteria like the Lachnospiraceae-Ruminococcaceae family and Roseburia species under Clostridium cluster XIVa, with Clostridium leptum and Fecalibacterium prazusnitzii significantly increased in the Goji group. Interestingly, the gene encoding butyryl-coenzyme A CoA transferase, crucial for butyrate synthesis in these bacteria, showed a sixfold increase in the fecal samples from the Goji group, correlating with higher fecal butyrate levels. This phenomenon indicates that Goji berry's dietary inclusion results in Bifidobacteria proliferation and the butyrate-producing bacteria's blooming, which may have cross-feeding relationships providing preventative effects against colitis.
A Randomised Controlled Trial published in 2017 in the journal Nutrition and Healthy Aging found that Carrageenan intake can lead to an earlier relapse in patients with ulcerative colitis who are in remission. In the methods employed, a clinical trial was carried out to determine if ulcerative colitis patients could avoid or defer relapse by following a diet devoid of carrageenan. Participants were educated about the no-carrageenan diet, and then divided into two groups - one receiving capsules containing carrageenan and the other receiving placebo capsules. The amount of carrageenan in the capsules was less than the average daily dietary intake. Relapses were defined by a rise of two or more points on the Simple Clinical Colitis Activity Index and the need for enhanced ulcerative colitis treatment. Over the course of a year, participants were monitored every two weeks via phone calls. In the research results, it was found that out of twelve patients, those who ingested carrageenan capsules had a higher relapse rate. Notably, none of those who took the placebo experienced a relapse. The group exposed to carrageenan exhibited increased levels of inflammation indicators - the Interleukin-6 and the fecal calprotectin biomarkers - by the end of their participation in the study. There was no such increase observed in the placebo group.
Moderation Tools
Topic
Sign In
Users not signed in are limited to viewing the 5 most recent items of content.